Project Grant 2018
Tissue-crosstalk and Metabolic Regulation of Type 2 Diabetes
Principal investigator:
Juleen R. Zierath, Professor of Clinical Integrative Physiology
Co-investigators:
Karolinska Institutet
Per-Olof Berggren
Carsten Daub
Anna Krook
Erik Näslund
Mikael Rydén
Swedish University of Agricultural Sciences
Thomas Moritz
Institution:
Karolinska Institutet
Grant in SEK:
SEK 18 million over three years
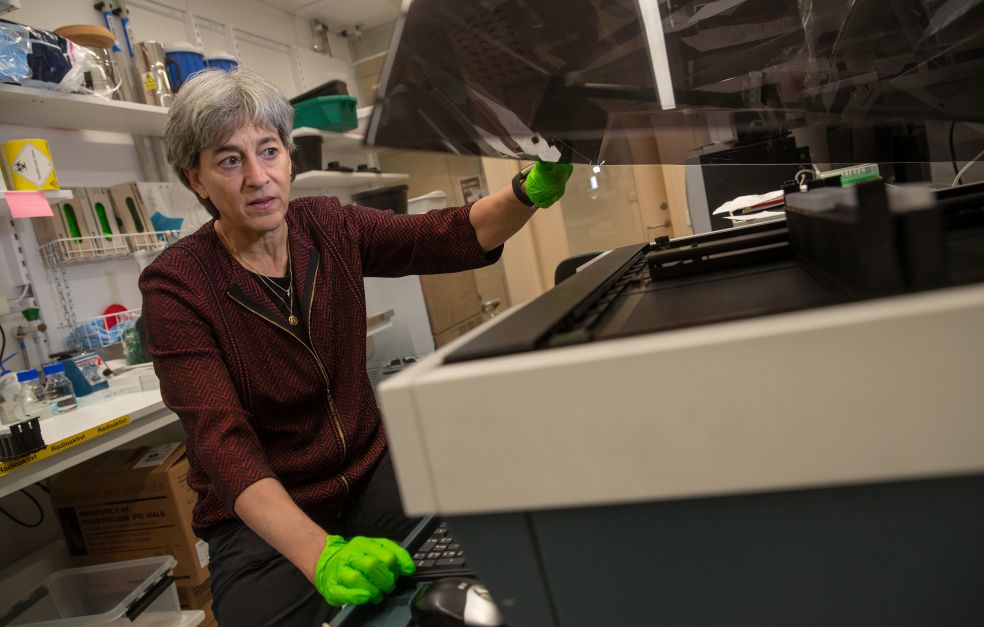
“Here we are preparing liver samples. We’re trying to understand how a protein secreted by the muscles affects the liver in mice,” says Zierath, Professor of Clinical Integrative Physiology at Karolinska Institutet.
The research in this lab aims to learn more about type 2 diabetes, the most common form of diabetes. The work is taking place in a project funded by Knut and Alice Wallenberg Foundation, which brings together six research teams from Karolinska Institutet and one from the Swedish University of Agricultural Sciences.
Type 2 diabetes can be caused by a malfunction of the so called beta cells in the pancreas that produce insulin. The body can also fail to respond normally to insulin, which is called insulin resistance. Insulin is a hormone needed by the body to remove sugar from the blood.
The exact cause of type 2 diabetes is unknown. Certain genetic variants increase the risk of developing the disease, but lifestyle factors such as obesity and a lack of exercise also play a major part.
How organs talk to each other
The researchers are examining the interaction between the organs that play a key role in regulating the body’s blood sugar level – fat, liver and skeletal muscle.
“We want to know how these organs talk to each other, and how this affects the health of the insulin-producing beta cells, and the body’s insulin sensitivity,” Zierath explains.
People with type 2 diabetes often suffer from low-grade chronic inflammation, i.e. an inflammation that is constant, but does not trigger clear symptoms. The inflammation causes the cells to release substances that interfere with the interaction between the organs regulating blood sugar. The researchers want to understand this better.
“Our hypothesis is that substances released from fat, skeletal muscle or liver impair the function of the beta cells during the onset of type 2 diabetes,” Zierath says.
The researchers are particularly interested in the release of metabolites – molecules formed during cell metabolism. They are studied using metabolomics, which maps all metabolites in a given tissue at a given moment. The researchers will be studying metabolite patterns in organ samples from healthy control subjects, and comparing them with samples from people with diabetes. The aim is to understand how metabolites transmit information between the organs and play a part in the progress of the disease.
The huge quantity of data from the metabolomics studies is one of the challenges faced in the project. Zierath explains:
“We have to filter it down to a manageable number of metabolites worthy of further study. We don’t know if it will be a single metabolite, or several in combination, that produce an effect, or whether we will obtain a high enough resolution to determine the importance of an individual metabolite.”
Experimenting on cells and live animals
In the cell culture laboratory Zierath puts a flask containing muscle cells back in the incubator. A key element of the project is to examine how the metabolism of cultured cells is impacted by the addition of different metabolites. The team is studying how glucose uptake changes, for example. They are also using animal models to study the effect of various metabolites, and to examine the function of beta cells in living animals.
The project requires cutting-edge expertise in multiple fields. Alongside Zierath, who specializes in studies on skeletal muscle from animals and humans, the team includes researchers with expertise in beta cells, fat cells, liver cells and metabolomics.
“One advantage of these grants is that they are large and daring, and can bring researchers together in pursuit of a common goal,” Zierath comments.
So far, one of the co-investigators, Mikael Rydén, Professor of Clinical and Experimental Adipose Tissue Research at Karolinska Institutet, and colleagues, have seen interesting effects caused by one metabolite. They have found that fat cells from healthy individuals release more of the metabolite than those from people with insulin resistance, and that the metabolite reduces inflammatory signals from the fat cells.
Experiments using cultured muscle cells showed that the metabolite also reduced inflammatory signals from those cells. So the researchers decided to move on to mice, which were given either the metabolite or a control substance over a two-week period.
“The mice given the metabolite metabolized glucose slightly better and lost weight. We now intend to investigate this further,” says Anna Krook, Professor of Integrative Cell Physiology at Karolinska Institutet.
Healthy food
One hope is that the project will result in markers capable of identifying people with a high risk of developing type 2 diabetes. Ultimately, the researchers envision this knowledge being used to develop new healthy foods.
“If we succeed in demonstrating that certain metabolites have a positive effect, they could be added to food and drink to delay the onset of type 2 diabetes,” Zierath says.
Text Sara Nilsson
Translation Maxwell Arding
Photo Magnus Bergström