Project Grant 2013
Novel treatment of advanced melanoma by targeted pro-senescence therapy combined with immunotherapy
Principal investigator:
Lars-Gunnar Larsson, Professor of Tumor and Cell Biology
Co-investigators:
Johan Hansson
Rolf Kiessling
Galina Selivanova
Margareta Wilhelm
Klas Wiman
Institution:
Karolinska Institutet
Grant in SEK:
SEK 33.6 million over five years
Hot sun in the garden, at the outdoor restaurant and on the sandy beaches. Swedes are a sun-worshiping people and gladly shed their clothes as soon as the sun peaks through the clouds. And sunbathing has some good health effects. The sun stimulates the body's production of vitamin D, which is linked to better protection against prostate cancer and some other kinds of cancer. But the extensive sunbathing of today also has a serious downside, according to Lars-Gunnar Larsson, Professor of Tumor and Cell Biology at Karolinska Institutet.
“In earlier times, people had on clothes and hats in the sunshine and farmers who worked out in the fields protected themselves well. Now, people can lie on the beach without much clothing for hours, a behavior that explains the increase of melanoma.”
Constant mutations in skin cells
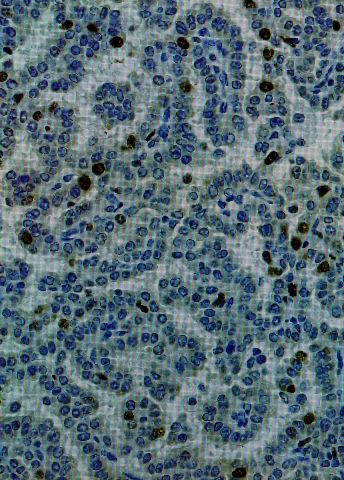
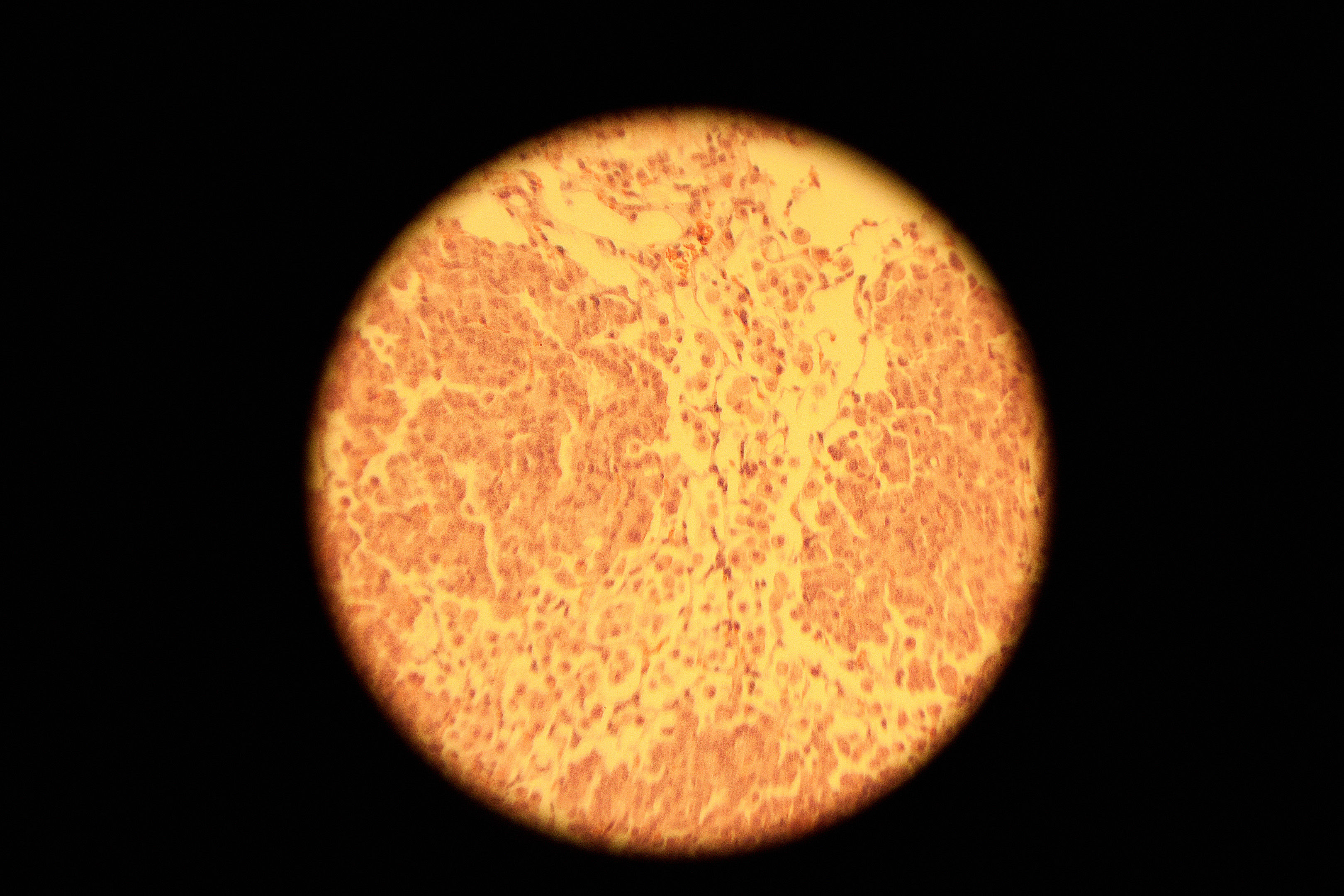
Skin cells have a high frequency of mutation, mainly due to the radiation from the sun. Most of the mutations are completely harmless, but if mutations take place in the cancer genes BRAF or RAS, benign tumors begin to grow, so called nevi or moles, which further on can develop into malignant melanoma.
However, the cells have their own defense mechanisms against such events. They can divide a certain number of times, but after that, the cell crashes in a condition called senescence, which means that the cell permanently stops dividing. Various defense mechanisms are activated that keep the cell from dividing further.
“It becomes a ‘dead end’ that means that a tumor cell cannot continue to grow,” says Lars-Gunnar Larsson.
But sometimes, something happens that allows the cell to succeed in outsmarting the senescence mechanism. The defense system stops working and the benign tumor converts into a harmful, malignant tumor. One such event is the activation of the Myc gene.
Regular cancer gene involved
Over the years, Lars-Gunnar Larsson has become a specialist on Myc, which is an opponent of the known anti-cancer gene p53 and, like p53, is involved in many kinds of cancer. Myc’s main task is to keep cells dividing. For example, if a cell needs to divide during embryonic development or to replace worn out cells at an adult age, the command comes from signals that activate Myc. Myc controls 10 to 15 percent of all genes in the human genome, all of which are needed for cell growth.
When senescence occurs, the phase in which the cell stops dividing and all growth stops, Myc is turned off. This is completely normal. But if the cell nonetheless keeps dividing, it may be because the defense system failed to turn off Myc. This means that yet another mutation has occurred and a tumor suppressor has been disabled that otherwise would keep Myc under control. The process continues and is at risk of making the transition over to invasive cancer, an aggressive disease phase.
Larson and other researchers have been able to show in animal models that tumor cells are often absolutely dependent on Myc. If Myc is turned off or if p53 is activated, the cells immediately stop growing and the senescence condition is again achieved.
Hope for new medicines
To take advantage of the new knowledge, six researchers at Karolinska Institutet, specialized in skin cancer, immunology, the Myc gene and the p53 gene, will collaborate in a project financed by the Knut and Alice Wallenberg Foundation.
They are now working on finding various ways of turning off or inactivating Myc and it is hoped that a medicine that inhibits Myc will be able to be developed on the long term. Other researchers in the team are developing medicines that activate p53.
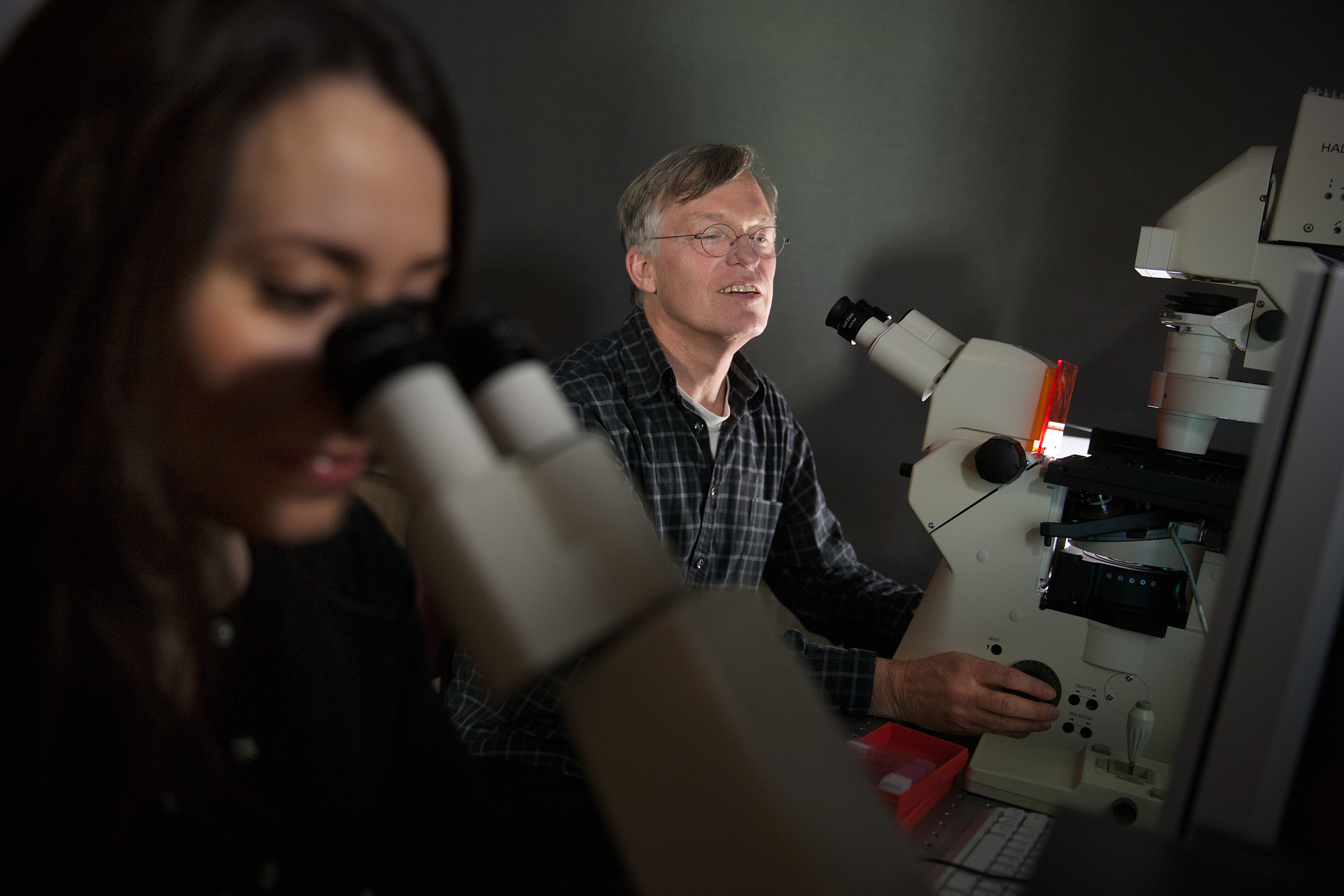
“Many cancer medicines are based on killing the actual tumor through programmed cell death. It feels safest, but unfortunately many tumors become resistant and refuse to die. The new treatment could be seen as a plan B. If the cell refuses to die, we say: ‘OK, if you won’t die, you can live, but can never divide’.”
The vision is that the future form of treatment, which has been labeled senescence therapy, will be able to be combined with the tailor-made, targeted therapies that have been developed against the BRAF gene in recent years and have been successful, but where there is currently a problem with the development of resistance.
One of the main ideas of the project is that senescence therapy will be able to interact with immunotherapy, which seeks to stimulate the body’s own immune system to fight the tumor cells. The senescent cells have the characteristic that they emit molecules that attract immune cells. The immune cells can in turn kill tumor cells that have become resistant to treatment. In such a case, there would never be a need to fear the risk that the tumor cells wake up again from their dormant senescent state.
“It is an attractive thought to use several different approaches be able to achieve a truly effective treatment. If we succeed in locking in the tumor cells and blocking three escape routes at the same time, it should at least theoretically be difficult for them to spread, but this remains to be proven,” says Lars-Gunnar Larsson.
Text Nils Johan Tjärnlund
Translation Semantix
Photo Magnus Bergström
Facts about malignant melanoma:
The sun’s ultraviolet radiation causes damage in the cells genetic material.
The cells that create the brown pigment that blocks the ultraviolet radiation are called melanocytes. I
t takes more time for lighter skinned people to build up a protection, while darker skinned people most often have a natural protection.
Sometimes, the sickness arises in regular liver spots or moles, but it can also begin directly in the skin.
Malignant melanoma can occur anywhere on the body.
Women most often get the disease on the lower legs and men on the upper body.
Common initial symptoms are a birthmark (nevus) that begins to grow, itch, bleed or change shape and color. New changes that did not previously exist can also arise.
There are also other kinds of skin cancer.
Basal cell cancer grows from cells in the basal cell layer. This disease most often occurs on the face, but can also occur on the upper body.
Pavement epithelium cancer radiates from the middle layer of the upper skin or from deeper skin layers. This skin cancer is most often found on the parts of the skin that are most exposed to the sun, i.e. the face, the outer ear, the back of the hand or a bald head.