New technology allows detailed mapping of cancer cell DNA. Thoas Fioretos and his colleagues are looking for unique features of the cells that may lead to new diagnostics and less grueling therapies.
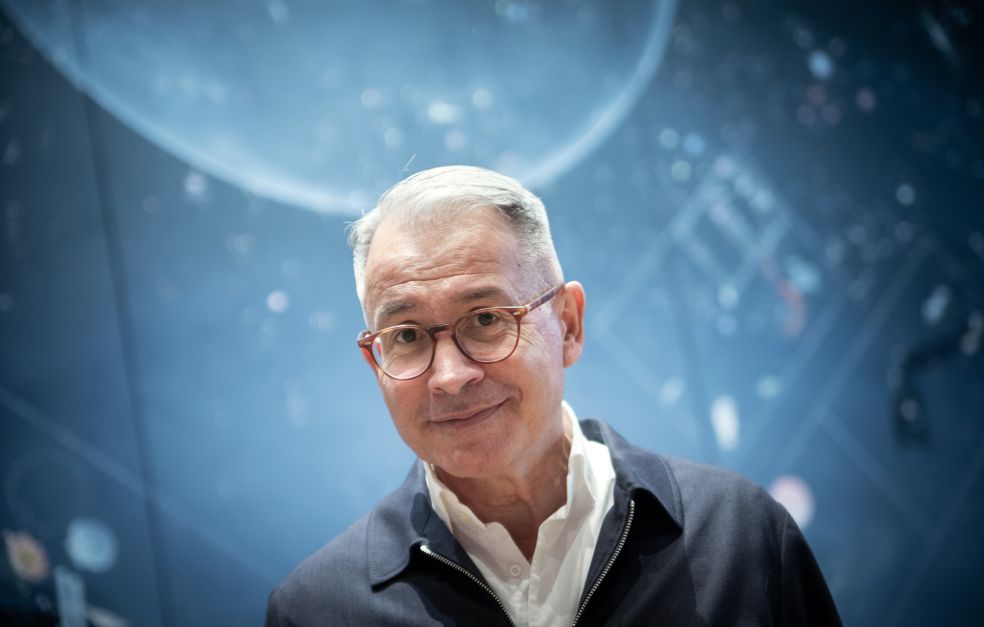
Thoas Fioretos
Consultant and Professor of Clinical Genetics
Wallenberg Clinical Scholars, prolongation grant 2023
Institution:
Lund University
Research field:
Acute leukemia, cancer genetics
Thoas Fioretos is a consultant, professor of clinical genetics and a Wallenberg Clinical Scholar at Lund University. He is researching acute forms of leukemia – blood cancer – that are linked to numerous changes in cell DNA.
“If we identify changes that are important and why this is so, we may be able to develop better diagnostics and new therapies.”
Fioretos’ team is focusing on genetic variations that cause changes on the cell surface. Proteins are found there that act as receptors for various substances and may differ between diseased and healthy cells. The researchers are using experimental models to ascertain whether a given receptor is key to cancer cell survival and if so, whether it can be blocked, usually by means of an artificial antibody that can then form the basis for a new therapy.
Current therapies effective but grueling
Some of the findings are put to use straight away in the form of more accurate diagnosis. The group has discovered a genetic change that explains between five and eight percent of all cases of childhood leukemia, and is used for diagnostic purposes. But as yet there are no targeted therapies for children with this form of leukemia. The researchers have bred genetically modified mice with the gene variant so they can examine it, and compare the efficacy of existing drugs.
“At present 95 percent of all children with leukemia are cured, which is fantastic. But it’s an extremely grueling treatment that can cause long- and short-term side-effects. Pure scientific research is enormously interesting, but I also want our discoveries to make a difference,” says Fioretos.
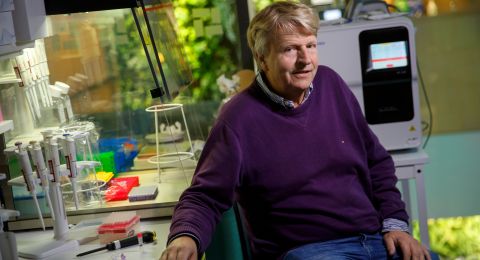
New technologies play a key role in cancer research. Sequencing machines that map DNA sequences and detect changes have recently become faster, and examinations less costly and more accurate. Another innovation is single-cell analysis, which enables scientists to study the DNA of thousands of individual cells.
“Sifting through and sorting out the huge quantities of data we generate is a huge job. The new grant will enable me to recruit two mathematicians to the team to carry out data modeling.”
I believe this to be the diagnostics of tomorrow: genetic patterns that show us the best way to treat a patient.
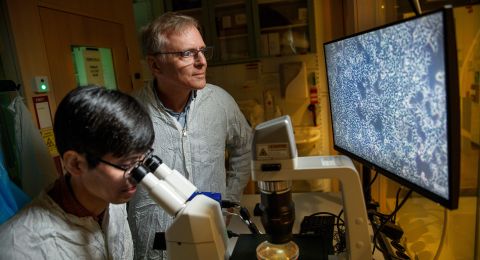
Cancer stem cells in hiding
One key target is cancer stem cells – “mother cells” that create the other cancer cells. They make up only a tiny proportion of the total quantity, but the researchers can study them using single-cell analysis and flow cytometry. If they find unique structures on the surface of the stem cells, it may be possible to develop antibodies to knock them out, thereby eliminating the cancer completely.
Fioretos’ team has found two such surface molecules in leukemia patients. One of them is normally found only in immune cells. When the researchers in the laboratory removed the molecule, immune system T-cells began to attack the cancer stem cells. The research team has also found the same molecule on the cell surface in tumors, which have nothing to do with the blood system.
“Our hypothesis is that this is a way for the leukemia stem cell to disguise itself and fool the immune system, and that this is a fairly fundamental mechanism. If we learn more about it, it may be of help in treating other forms of cancer.”
Good to combine clinical work with research
As a professor and consultant, Fioretos spends some 70 percent of his time on research, and the remainder on clinical work. He is responsible for the sequencing-based diagnostics for leukemia, attends multidisciplinary conferences, reports analytical findings to cancer doctors, and provides patients with genetic guidance.
“Sometimes I research things I see when I send out analysis responses, and sometimes during my clinical work I see details I wouldn’t have noticed if I hadn’t done research. This is valuable. But these days I see fewer and fewer doctors who have the time and opportunity to research, and fewer researchers working in health care. This worries me. The research of today is the health care of tomorrow, but I see that Sweden, having been one of the leading countries in clinical research, has begun to lag behind.”
A patient study in the U.S. based on Fioretos’ team’s findings is due to start soon. The study concerns a surface molecule that the team has identified and developed an antibody for. A company has been set up in the southern Swedish city of Lund to develop the antibody. A clinical study involving leukemia patients will now be conducted at MD Anderson Cancer Center i Texas, one of the highest-ranked cancer hospitals in the U.S. Patient samples will be analyzed by Fioretos and his colleagues in Lund.
“It’s really exciting that our discovery is resulting in a study at one of the foremost cancer hospitals in the world, and that we are taking part by examining the impact on cancer cells – it completes the circle.”
Within a few years he hopes to proceed with antibodies for more forms of leukemia. He expects the process to be speedier thanks to new technology and knowledge.
“I truly never have a boring day at work. And it’s very satisfying to know that what we’re doing offers the potential for better therapies. I never need to ask myself whether what I’m doing is important.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Åsa Wallin