Project Grants 2011
Genes to function, autoimmune diseases
Principal investigator:
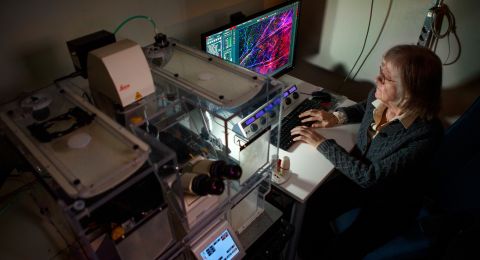
Ann-Christine Syvänen, professor of molecular medicine
Co-investigator:
Lars Rönnblom
Institution:
Uppsala University
Funding in SEK:
23.8 million over five years
In recent years Ann-Christine Syvänen and her colleagues have found genes that are risk factors for SLE, and now their research is moving on to study how these genes function at the molecular level in order to elucidate the causes of the disease.
Some 6 000 Swedes suffer from SLE. It is a chronic autoimmune rheumatic disorder that can affect virtually all organs in the body. The kidneys, heart, lungs, central nervous system, and blood vessels can be attacked.
Some patients get the red butterfly-like rash across the nose and cheeks that has given the disease its name. Lupus erythematosus means "red wolf-bite" in Latin.
“It’s a very serious disease,” explains Ann-Christine Syvänen, who is professor of molecular medicine at Uppsala University.
“SLE occurs in many different forms and can be very difficult to treat. It’s a systemic disorder, and virtually any organ in the body can be affected. This is also why SLE is regarded as a model disease for autoimmune diseases, which makes this research interesting in a wider perspective.”
The disease is probably caused by a complex interplay of heredity and environment, but the hereditary component is very high, about 70 percent according to studies of twins. In recent years new genes have been identified as elevating the risk of developing SLE. It is now known that some 40 different parts of the genome contain risk genes, and many of them were discovered by Ann-Christine Syvänen and her colleagues at Uppsala.
Unique patient material
These successful findings are based on access to a patient material that is a goldmine for Swedish medical research. The data is being collected within the framework of a national SLE network comprising researchers from all over Sweden and directed by Lars Rönnblom, professor and senior consultant at the Rheumatology Unit at Uppsala University Hospital. All in all, some 1 200 SLE patients have given their consent to having their samples used for research purposes. The material began to be collected ten years ago and is still being gathered.
“These Swedish samples are well characterized, using a consistent set of diagnostic criteria. This is extremely important when you conduct genetic studies,” says Ann-Christine Syvänen.
The identified genes probably have important functions in the immune system, and there have been some surprising discoveries. One of the genes identified, TNIP1, codes for a protein that also participates in a signal path with a key role in systemic inflammation. Moreover, the TNIP1 protein can cooperate with another protein whose gene is linked to several autoimmune diseases.
“We have also found other genes that are common to autoimmune disorders. They evince the complex interplay within the immune system found in many rheumatic diseases. Now, in the new project, we are going to start to study the function of these genes and chart how they are expressed. The aim is to look very carefully at the phenotypes, to classify them and see if we can distinguish different subgroups of SLE.”
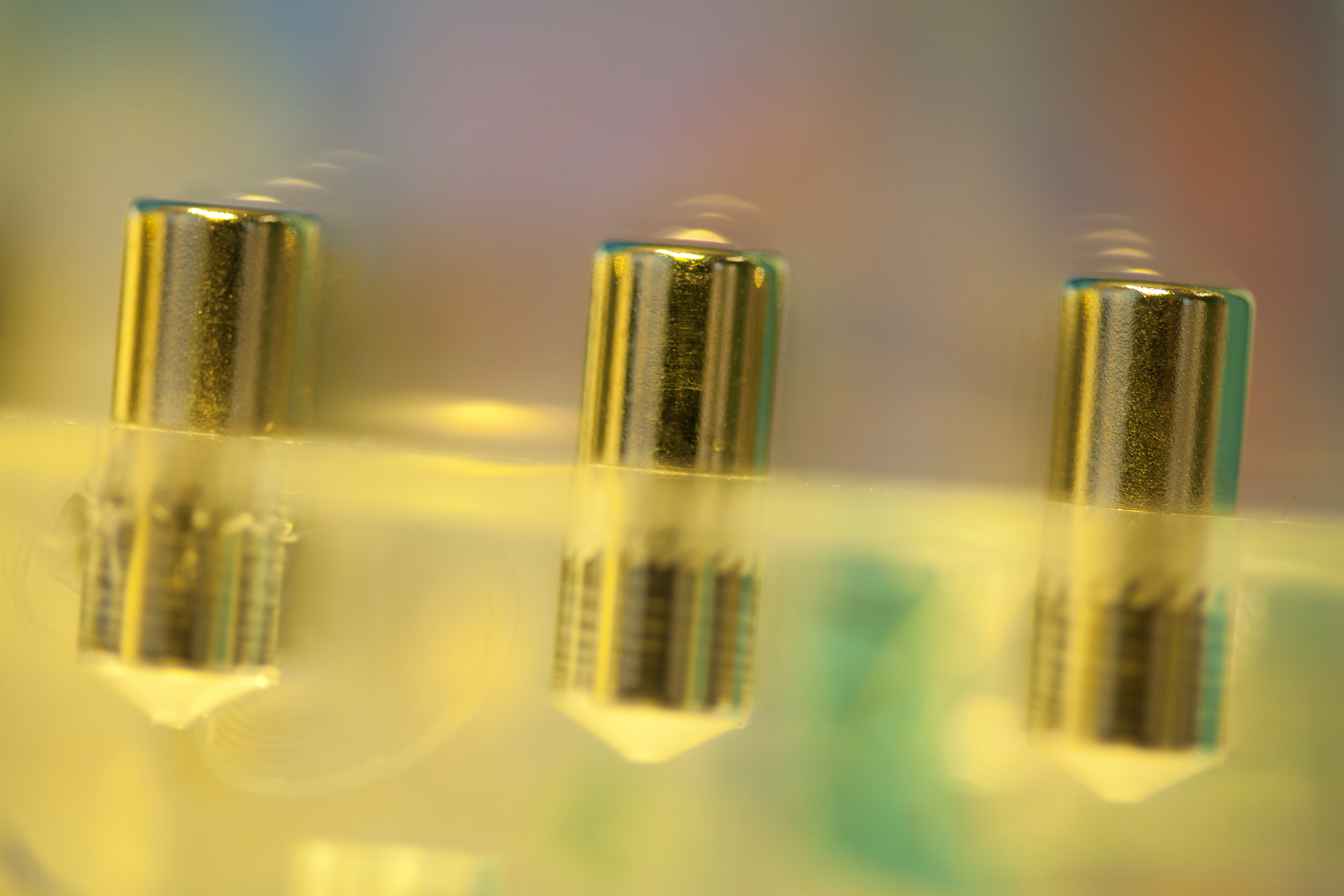
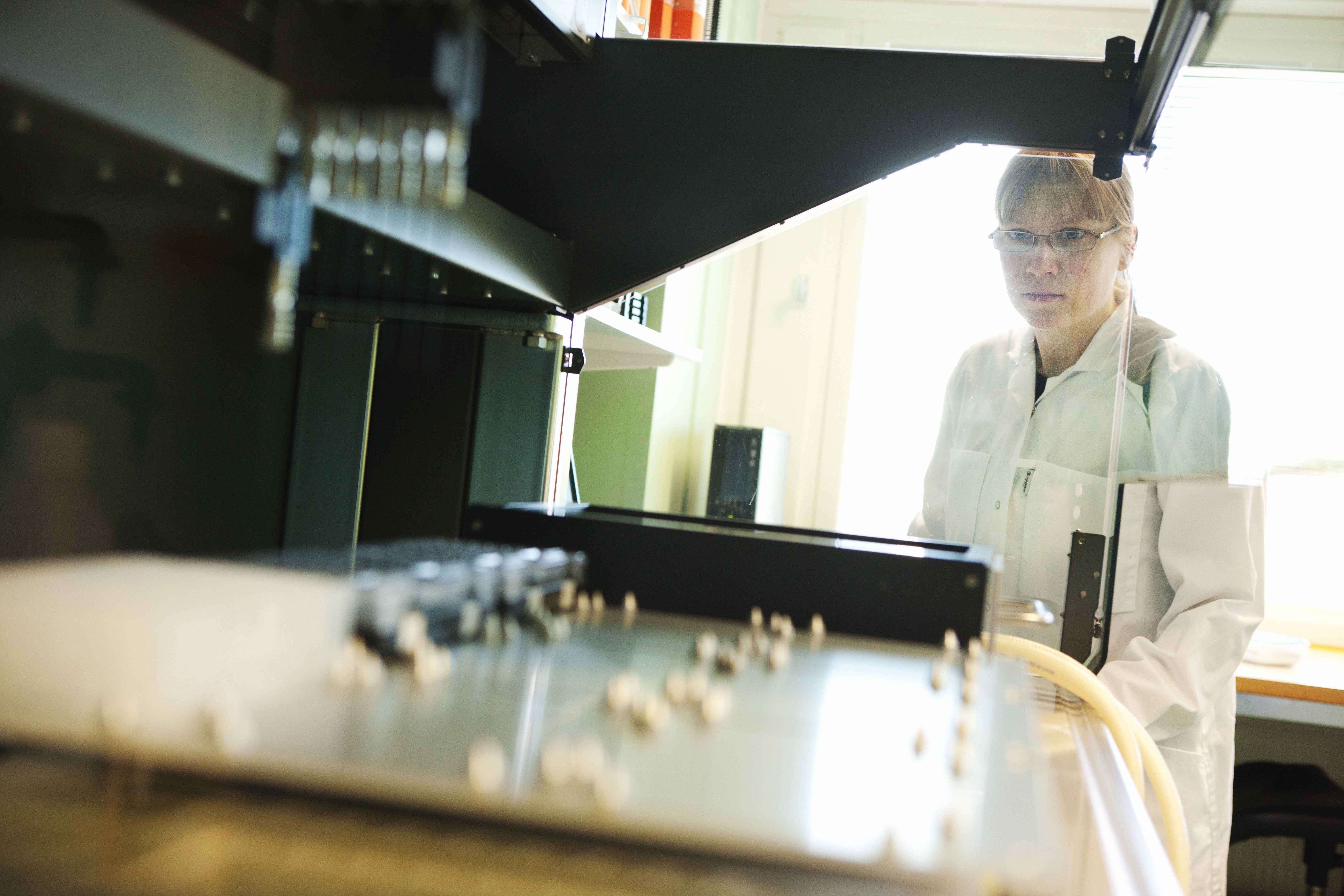
The researchers are creating a model system artificially in order to study the disease in detail. They isolate blood cells from healthy donors and fractionate the cells into different cell types. The cells are then treated with immune complexes that are similar to the situation in SLE.
“We’re trying to ‘ape’ SLE in blood cells and thereby find out what cell types are important in different phases, what genes are expressed, how they are regulated, and any possible epigenetic changes in the cells.”
Better treatment in the long run
Since the causes of SLE remain unknown, we will have to wait for new treatment methods. But the enhanced knowledge we have gathered in recent years nevertheless represents a number of steps forward. In 2011 a new biological drug was registered, based on antibodies against a growth factor for B-lymphocytes, which is one of the cell types that are key in the pathological process. But this treatment is very expensive.
In clinical trials a cytokine inhibitor is also being tested, targeting interferon, which is thought to play an important role in the disorder. Interferon is a protein that is secreted in connection with infections and helps stimulate the immune defense when we contract viral diseases, for example. In normal cases the production of interferon drops when the infection has left the body, but this shut-off doesn’t seem to function in pathological conditions like SLE. Instead it remains constantly active and triggers the immune defense to attack the body’s own cells.
The link to interferon was strengthened a few years back when Ann-Christine Syvänen was able to locate risk genes for SLE among the genes involved in the interferon system.
“But it’s a complicated connection, so we don’t expect to be able to design any new medicines in this project. The ambition is to create a better understanding of the fundamental mechanisms and to be able to provide new approaches to other autoimmune diseases as well. Maybe we can also create better prognostic tools for which patients run the risk of developing complications, such as stroke.”
Text Nils Johan Tjärnlund
Translation Donald S. MacQueen
Photo Magnus Bergström