Project Grants 2011
Droplet microfluidics and functionalized nanowires for detection of circulating tumor cells
Principal investigator:
Jan Linnros, professor of materials physics
Co-investigators:
KTH
Amelie Eriksson Karlström
Helene Andersson-Svahn
Joakim Lundeberg, Afshin Ahmadian
Uppsala University
Shili Zhang
Karolinska Institutet
Rolf Lewensohn
ACREO
Christian Vieider
Per Björk
Institutions:
KTH in collaboration with Uppsala University, Karolinska Institutet and ACREO
Funding in SEK:
More than SEK 33 million over five years
The project, which is being funded by the Knut and Alice Wallenberg Foundation, is focusing primarily on finding tumor cells that cause lung cancer. The method can be used both to see whether the cancer has spread and formed metastases and to see if there are lingering cancer cells after treatment.
“You could possibly also see what kind of tumor it is. This means you can administer a treatment that is custom-designed for that type of cancer. In ten percent of patients where cancer is suspected, no tumor is found. But using this method it will be possible to see whether they have tumors and what type they are,” explains Jan Linnros.
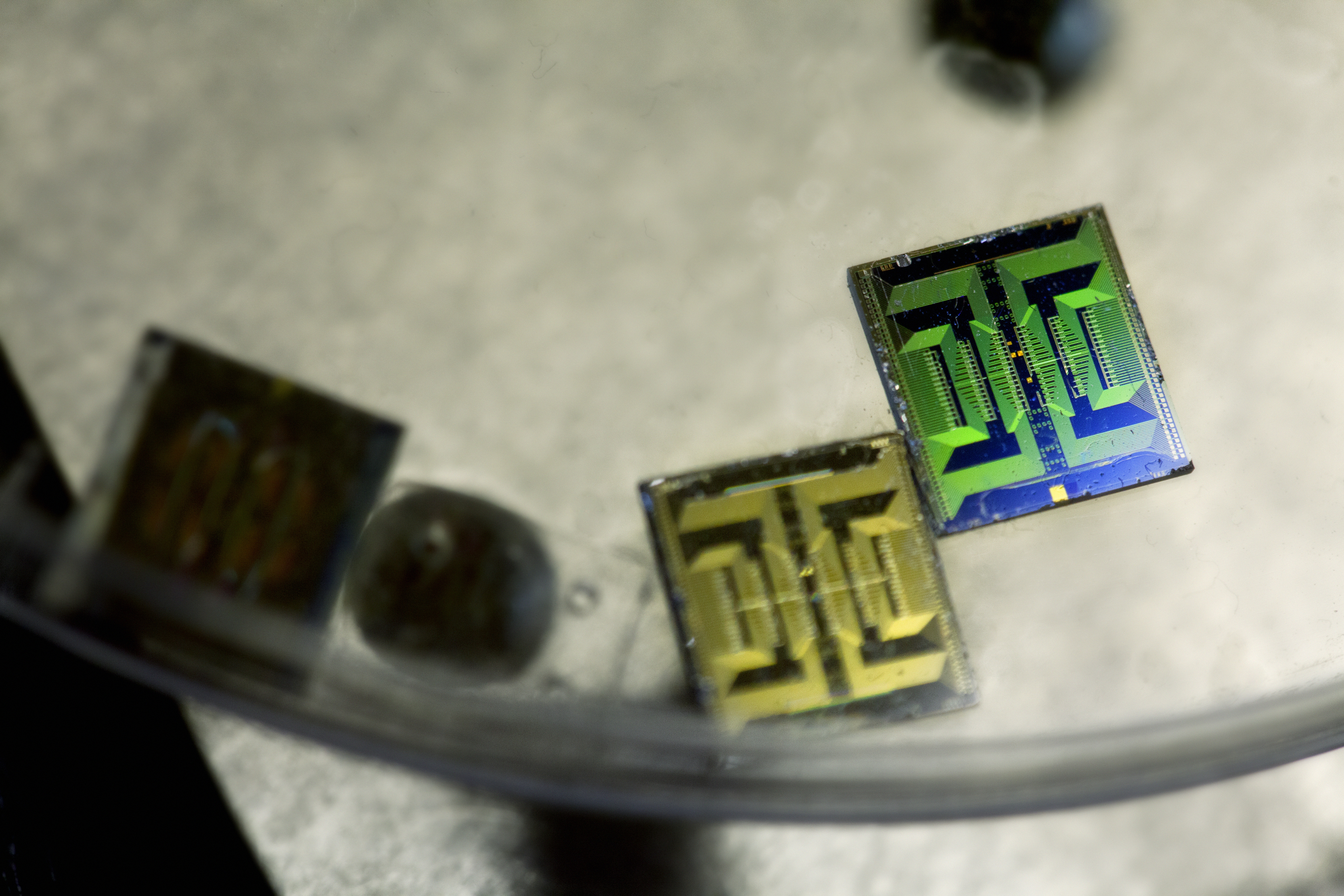
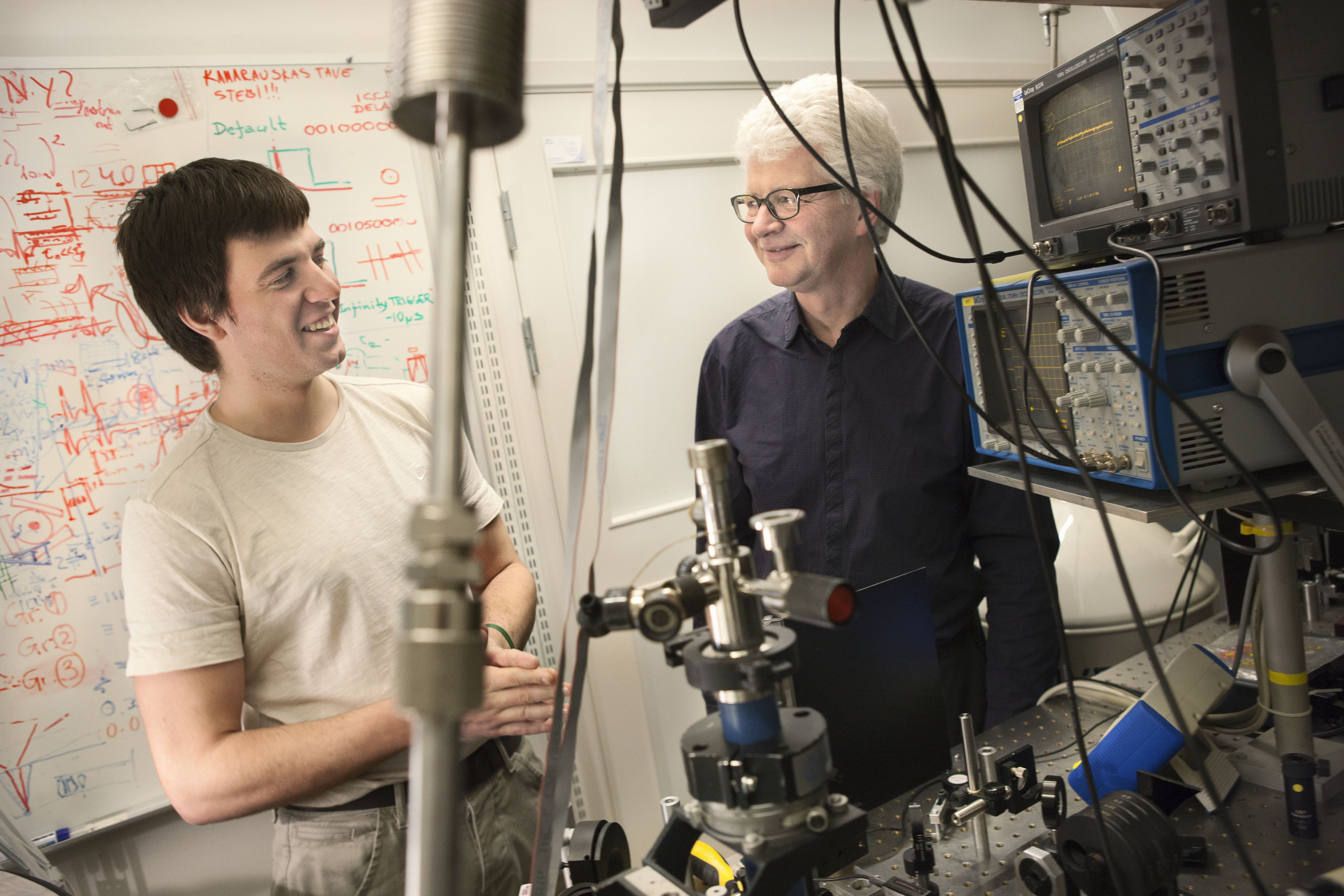
Microchip detector
Jan is professor of materials physics and has his lab at KTH Royal Institute of Technology in Stockholm. But in this project he is also working with chemists, biotechnologists, medical researchers, and electronics researchers at the Karolinska Institutet, Uppsala University, and the research institute Acreo. Altogether about 30 researchers are applying their expertise to the task of creating a microchip and a method that can discover and detect circulating tumor cells.
“We have put together a team to cover the whole chain, including an oncologist. The microchip is basically already completed, but now it’s a matter of getting its recognition and functionality to match what we want it to detect,” says Jan Linnros.
By the end of the project, in 2016, they hope to have a functional method.
“Many different technologies need to be brought together to form a functioning unit. Biotechnology in combination with surface chemistry and physics is never simple, so we don’t know whether it will work the way we thought, but we hope so. Nor are we absolutely certain that tumors are spread by circulating cancer cells, although most of the evidence indicates this,” says Linnros.
Sensitive nanowires
A cancer tumor can spread to other organs or tissues via blood. This spreading probably occurs when cancer cells enter the blood circulation. Thus, with a simple blood sample, it should be possible in principle to measure the spreading activity of a tumor.
“The problem is that among 100 million cells, five circulating cancer cells may be hidden. This means you have to have a method that is certain to detect them,” says Amelie Eriksson Karlström, professor of molecular biotechnology, KTH.
“The microchip contains nanowires, among other things. By placing antibodies on the wires, we can detect the biomolecules that come from the cancer cells we’re looking for.”
“The nanowires are so tiny that they have an extremely sensitive surface. When you run current through them, you can see from the changes in the current whether you’ve captured the right biomolecules,” explains Linnros.
The effect is a result of simple electrostatic attraction or repulsion of the electrical charges in the nanowire, and the corresponding change in resistance, depending on the charge of the captured biomolecules.
“We can also construct a chip with different nanowires and antibodies in order to detect several different biomolecules at the same time and get more information about cell content. Besides proteins, we can detect DNA filaments and monitor the expression of genes,” says Linnros.
“We hope the method will teach us more about cells,” adds Amelie Eriksson Karlström.
Large quantities in short time
Amelie’s research team is busy finding molecules, antibodies, and other proteins that function as markers of cancer cells.
“Each protein is unique. That means we have to find the right markers that provide sufficient information about the cancer cell. To know for certain that our robots are deploying them in the right place on the nanowires, we later put color markers on the proteins. In the microscope we see them as tiny luminous dots,” she says.
Another research team is working with droplet-based bio analysis. This is a system where each test cell consists of a microscopic droplet of water in oil. Since it’s possible to create and deal with some 10 000 droplets per second, the scientists are able to analyze huge numbers of cells in a short time.
“In this way we can fish out the cancer cells and measure and analyze them. If we can measure ten to twenty different proteins, we’ll see a genetic expression, a pattern that looks something like a barcode, and then we can tell what type of tumor we’re dealing with,” explains Jan Linnros.
Multiple applications
The sorted cells are each injected into their own droplet of water and placed in an oil-filled channel on the chip. The cells are counted, punctured, and emptied of their contents. The solution is then run past the nanowires, which are powered at a constant voltage.
“The nanowires react to the changes in the charge, and the result is a series of measurements that can determine the identity of each cell and perhaps its relation to the parent tumor.”
The researchers hope the technology for detecting biomolecules with nanowires will be so general that it will also be suitable for use in the food and pharmaceutical industries.
“If we succeed we’ll have a simple, inexpensive, and very rapid method,” say Jan Linnros and Amelie Eriksson Karlström.
Text Carina Dahlberg/KAW
Translation Donald S. MacQueen
Photo Magnus Bergström