Just over one in two hundred people in Sweden live with IBD – inflammatory bowel disease. Many of them get no relief from the drugs that are available. Eduardo Villablanca is studying the complex interactions of immune cells, intestinal cells and gut flora, to learn more about the causes of the disease and what can be done about it.
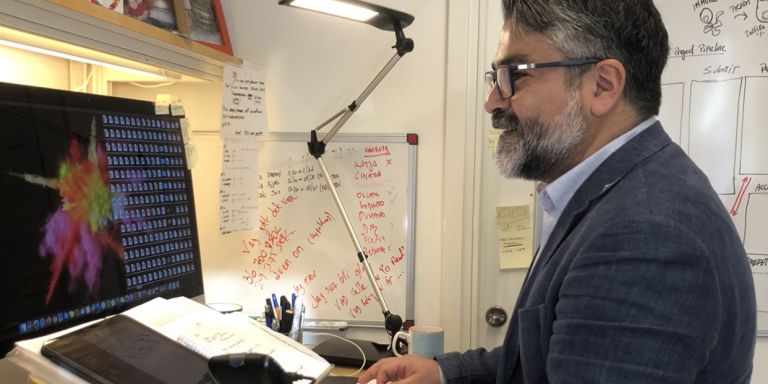
Eduardo Villablanca
Associate Professor of Immunology
Wallenberg Academy Fellow, prolongation grant 2019
Institution:
Karolinska Institutet
Research field:
Inflammatory bowel diseases; the intestinal immune system
The immune system in our intestines has an uncommonly difficult task. The body has to protect itself against alien bacteria and toxins, while tolerating and interacting with a wide variety of foods, and with several billion intestinal bacteria. If the delicate balance between protection and tolerance is disturbed, the immune system may react to the body’s own bacterial flora. This is a probable cause of IBD, of which ulcerative colitis and Crohn’s disease are two of the most common.
“There is no cure at present, IBD is a chronic condition. We can use drugs to keep it under control in some patients, but not all. I’m trying to understand how it occurs and what we can do about it. I’ve split my lab into two parts to study those two different aspects,” says Villablanca, who is a Wallenberg Academy Fellow at Karolinska Institutet.
Inflammation seen in zebrafish
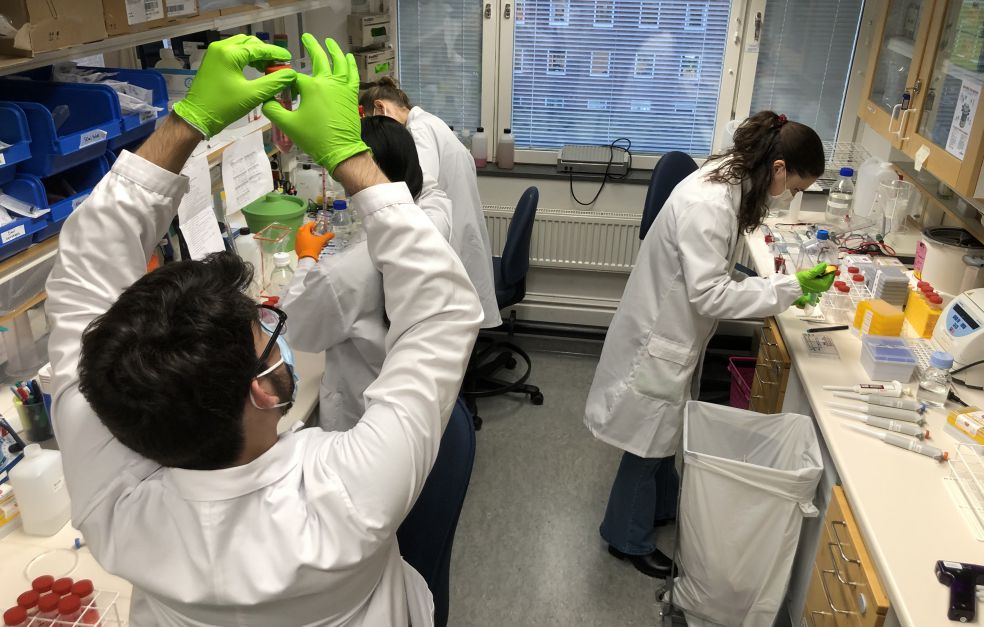
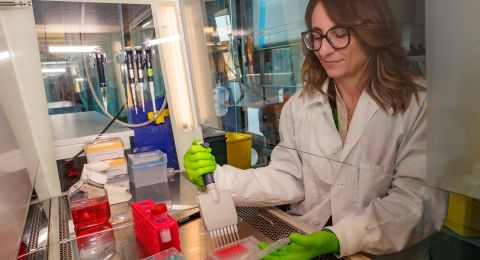
Since the disease is believed to be caused by a combination of genetic and environmental factors, he has designed experiments to study the interaction between individual genes and thousands of substances. He uses zebrafish, which have several advantages: they are small, easy to genetically modify, and are also transparent.
“Many factors can be involved in causing the disease, and it’s difficult to compare in mammals. The best approach is to screen the complex interaction between genes, immune cells and substances in living animals. This can be done with zebrafish.”
The fish have been genetically modified so that green or red color marks inflammatory substances called cytokines, or signs of intestinal damage. This makes the inflammation visible under the microscope, in the living organism. The researchers can then study the effect of activating or turning off different genes while adding chemicals, nutrients or intestinal bacteria.
“It’s often said that ‘genetics loads the gun; environment pulls the trigger’. And now we can visualize it as it happens,” Villablanca says.
Genetic sequencing – a potential step toward new therapies
One method he is using is single-cell RNA sequencing. The RNA in individual cells or areas in the tissue is mapped, providing information on the genes that are active in that specific cell or structure. This will give him a better understanding of the distinctive features of intestinal cells and immune cells in the various stages of the disease.
“We are developing a very comprehensive atlas of the process of intestinal inflammation and recovery, both in mouse and humans.”
His earlier research focused on dendritic cells – immune cells that process antigen material in the body and present it to the rest of the immune system. These days dendritic cells are only a small part of his work.
“The open-ended analyses we’re now making mean that we may end up studying virtually any cell type. After all, cells always interact with each other, so we must view intestinal processes holistically. The grant from Knut and Alice Wallenberg Foundation allows me to do just that.”
“The Wallenberg Academy Fellows is a fantastic scheme; I haven’t come across anything like it in other countries. It really pays dividends. I’m very grateful to be a part of it.”
A key finding was made in a study in which Villablanca compared laboratory mice that develop ulcerative colitis with humans suffering from the disease. This enabled him to see which genes were most significant, and then compare the activity of those genes in humans alone. He was able to identify two molecularly different groups, which he named UC1 and UC2. It turned out that more than half of the UC2 patients were helped by current drugs, whereas only one in ten UC1 patients benefited. He is now attempting to ascertain whether anything can be done to make group 1 more like group 2. This may be the first step on a long journey toward new drugs.
“Realistically speaking, it will probably take ten years before we can expect to try out something new on patients. During the first five years of my work there were many things we started but had to wind up because they didn’t work. This is unavoidable when you’re trying to break new ground. I’ve heard from the Foundation that they like failure. In that case I should be one of their favorites,” says Villablanca with a chuckle.
A problem-solving job
Villablanca grew up and studied in Chile. His father was a doctor. “Don’t study medicine,” he said. “If you want to make money from medicine, become a lawyer instead.” But Eduardo was fascinated by cells, genes and DNA. He wrote a master’s thesis on genetically modified zebrafish, moved to Milan to do his PhD, and on to the U.S. to work as a postdoc at Harvard Medical School and the Broad Institute. When his wife, who is Spanish, was working in Sweden, he was invited to give a visiting lecture. As a result, he was recruited to Karolinska Institutet. He has consistently pursued the lines of research he has found to be of greatest interest.
“I hate routine – I can’t stand it. I really wanted a job where I had to think and solve problems. As job that’s different every day.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Eduardo Villablanca