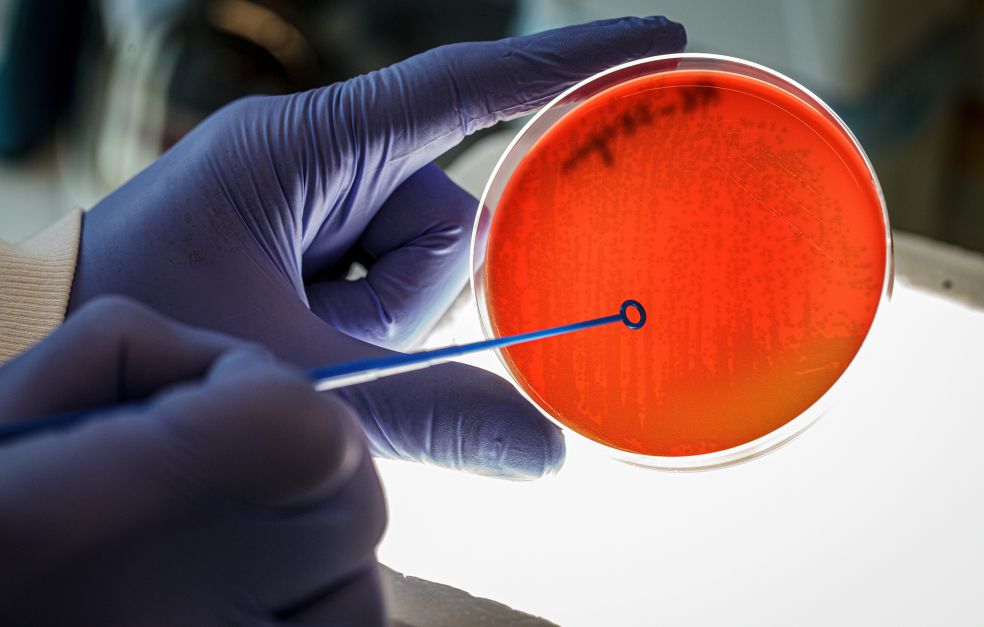
Pneumococci (Streptococcus pneumoniae) are bacteria that are common in the noses of healthy children, but they can also cause severe, even fatal, infections. Birgitta Henriques-Normark wants to find out why, and how we can reduce the risk of severe infections.
Birgitta Henriques-Normark
Professor and senior consultant in Clinical Microbiology
Wallenberg Clinical Scholar, prolongation grant 2023
Institution:
Karolinska Institutet and Karolinska University hospital
Research field:
Infectious diseases with a focus on respiratory tract infections.
Every year about two million people around the world die from pneumococcal infections. About 1300 severe cases are reported in Sweden annually. Many pre-school children have pneumococci in their nose without any symptoms at all; in other cases, the bacteria may result in sinusitis, ear infections, pneumonia, sepsis, or meningitis.
“Risk groups for severe infections are young children, the elderly, and those with deficient immune systems,” says Henriques-Normark, who is a professor and senior consultant in clinical bacteriology at Karolinska Institutet, and Karolinska University Hospital.
Since 2009, the Swedish vaccination program for children has included pneumococcal conjugated vaccines (PCVs), but these are only partially effective. Pneumococci have a sugar-based capsule, and it is the capsule that the vaccines target. Over one hundred different capsular structures have been identified, and the broadest PCV vaccine currently in use is based on twenty of them. But since the PCVs were introduced, pneumococci with capsules not included in the vaccines have increased dramatically causing severe infections. Moreover, the proportion of penicillin-resistant pneumococci has expanded.
Virtually anybody can get a pneumococcal infection, but some risk groups have been identified to be more susceptible to developing severe infections. There is much we still don’t understand.
Potential new vaccine using bacterial vesicles
As a Wallenberg Clinical Scholar, Henriques-Normark aims at understanding how pneumococci cause disease and finding better ways of preventing, diagnosing, and treating these infections.
For the moment her research team is working on a potential new vaccine. They have found that pneumococci release small vesicles surrounded by a membrane including pneumococcal proteins. The vesicles themselves do not cause infection, and the researchers have tested to see whether they could be used as a vaccine. They found that by injecting them in mice, the immune system reacts and builds up protection against pneumococcal infections.
“Our data suggests that we can reduce the risk of developing severe pneumococcal infection. It’s a completely different mechanism than current vaccines, and could protect against all pneumococci, not just certain variants,” says Henriques-Normark.
She is also examining how the disease-causing capability of pneumococci can be altered by their environment. The researchers have demonstrated that an infection with influenza virus causes more fluids to leak from the smallest blood vessels to the lungs thereby changing the environment in the lungs to promote pneumococcal growth. This is one explanation for why people are more susceptible to developing a severe pneumococcal infection after they have had an influenza virus infection.
Better diagnostics
Using powerful microscopes, genetic tools of various kinds, and animal studies on mice and zebra fish, Henriques-Normark and her colleagues are also engaged in a number of other projects. They are studying the toxin produced by pneumococci and found that it may inhibit the immune system, making it easier for the bacteria to survive. They are also examining the importance of pili: hair-like appendages found on the surface of bacteria. They were the first in the world to describe pili on pneumococci. They are also studying the effects of the restrictions that were implemented during the Covid-19 pandemic on the spread of pneumococci.
Their diagnostic projects are particularly important.
“We have developed a new, sensitive method of analyzing RNA in humans and in bacteria and viruses. We hope this method will enable us to identify new biomarkers that can be used as diagnostics to reveal whether a person has a severe pneumococcal infection or not. This is important since this will give us information on which antibiotic to give and avoid using antibiotics when they’re not needed.”
Twin roles beneficial
Henriques-Normark always knew she wanted to be a doctor. First, she planned to be a pediatrician, but some way into her studies she discovered microbiology and she worked for some time as an ear, nose, and throat doctor.
“I’m very curious, and keen on doing something good for humanity. If you want your research to make a real difference, you need to learn completely new things, such as the regulations governing development of new drugs, for instance. It’s a challenge, but it’s an important step to take.”
In her current position she devotes about two-thirds of her time to research. Her clinical work includes improving diagnostics and participation in the national surveillance program for monitoring pneumococcal infections and antibiotic resistance development in these bacteria in collaboration with the Public Health Agency of Sweden and Karolinska University Hospital. Henriques-Normark is convinced that her twin roles make her a better researcher.
“I combine clinical studies with basic research and identify important and clinically relevant research questions and attempt to answer them. At present, my main focus is on vaccine development, which is very exciting. This type of vaccine may also be used to target other bacterial infections. Additionally, we have found two molecules that have an antimicrobial effect. These could be developed into new antibiotics. We are in the process of exploring this finding.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström