A Swedish invention may revolutionize the treatment of fractures including fragmented bone injuries. The new method makes it possible to “patch” fractures with the help of a special glue. The vision for the future is that patients should not have to suffer the insertion of metal plates and screws.
Michael Malkoch
Professor of Fiber and Polymer Technology
Wallenberg Academy Fellow, prolongation grant 2017
Institution:
KTH Royal Institute of Technology
Research field:
Materials science, specializing in medical and biomedical applications
The bone adhesive is an innovation that may revolutionize the way surgeons mend fractures. Michael Malkoch, who is a Wallenberg Academy Fellow and professor at KTH Royal Institute of Technology, elaborates:
“Our methods are relatively non-invasive, reduce suffering and speed up the healing process,” he says.
Traditional methods such as steel or titanium implants can in the worst case do more harm than good. The body sometimes reacts negatively to the foreign materials. For example, over 40 percent of surgery to repair hand fractures using metal plates and screws has to be redone, which is costly for the health service and for the individual.
Moreover, there is a risk of new problems if the surgeon is later obliged to remove the implant for unforeseen reasons.
“The surgeon must then first free the implant from the soft tissue, tendons and new bone that have grown over it, which may result in permanent damage and new scarring.”
Problematic injuries
According to Malkoch, current solutions are clumsy. Some types of injury are almost impossible to treat using metal plates or screws. Finger fractures are one example.
“Human fingers are complex – they’re small, contain many tendons and perform advanced movements.”
Crush injuries are also difficult to treat – a crushed thighbone is a good example.
“Surgeons try to patch them up as best they can, but they have to leave some bone fragments alone. A loose piece of bone may later rub against soft tissue, causing intense suffering.”
But Malkoch now has a solution in his sights. For just over ten years he has devoted much time and effort to developing new technology that may lead to patient-specific treatment.
“We now have a bone adhesive that works and a new technology platform.”
Nobel Prize-winning concept
The research is based on click chemistry, a way of creating complicated molecules from simple building blocks. The concept is the brainchild of Barry Sharpless, who coined the term in the late 1990s. He was awarded the Nobel Prize in Chemistry in 2001 for another discovery, and is often mentioned as a potential second-time laureate for click chemistry.
Malkoch’s interest in click chemistry began during his time as a postdoc at Stanford University in California.
“Click chemistry can be used to solve materials research problems that are insoluble using traditional chemistry,” he says.
The difficulty was to produce an adhesive that is easier to control than current medical superglues. They are chemically uncontrollable and tend to stick together, whether to a liquid or a surface.
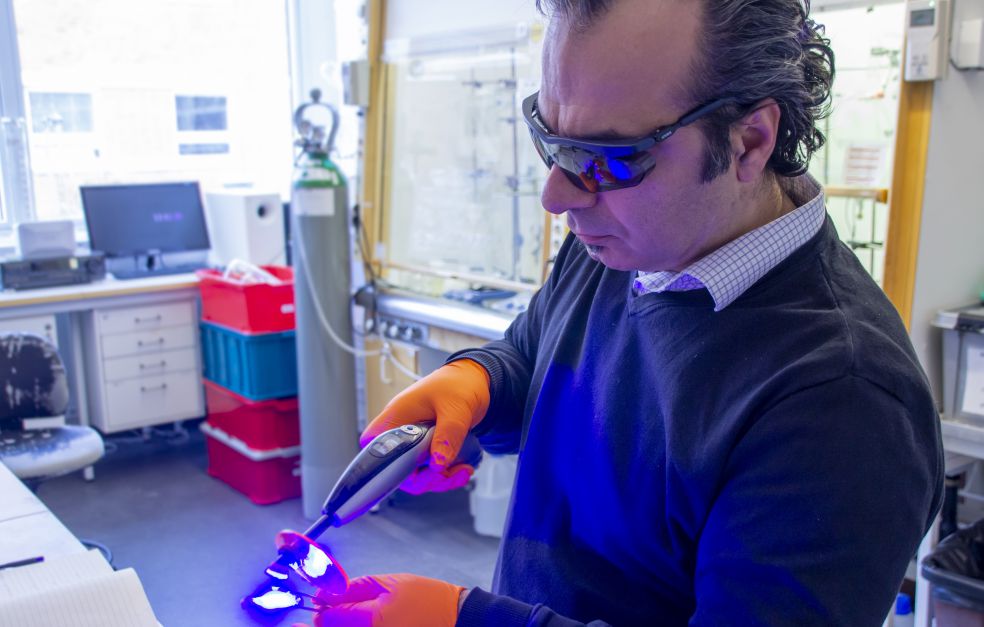
The new innovation is called bone adhesive, and consists of a fiber strip, a water-based primer and the adhesive itself. When surgery is performed the fracture is cleaned, the bone is primed and glued, and the fiber strip is then placed over it. More glue is then applied. An LED lamp is used to cure the material before further layers are applied and cured in the same way.
“The components are cured using a light, just like at the dentist. Studies have shown that our material gives 60 percent better adhesion than current dental glues. It’s also superior to steel wire and extremely stable.”
Malkoch emphasizes that the whole material is cured at once, unlike the process used to cure the composite materials currently used for dental fillings. When the chemistry is less robust, there is the problem that not all components are cured simultaneously.
“With post-curing the filling material shrinks, forming minute cavities in which caries can take hold, creating new problems. It is therefore essential that all curing take place rapidly.”
Successful results in animal models
In recent years trials have been carried out successfully using animal models. The next step is to develop the studies on human substrate, which is a time-consuming and costly process. In parallel, work is under way to commercialize the research and attract investors to fund clinical studies.
“I enjoy combining the roles of researcher and entrepreneur. Maybe I have inherited an entrepreneurial gene from my Lebanese origins,” Malkoch comments.
“The Wallenberg Academy Fellow grant is a mark of quality of my research. There is no doubt that the Wallenberg name opens international doors and makes it easier to build networks. The funding has given me the freedom to adopt an expansive approach and has enabled me to achieve something unique.”
The aim is to continue scaling up the platform so it can eventually reach different parts of the health care system. Other methods are also being used alongside the bone adhesive, including 3D-printed implants made from the body’s own tissues, and antibacterial materials in the form of hydrogel, which can be administered to combat multi-resistant bacteria.
There is a great need for better therapies, particularly for older patients. Brittle bones – osteoporosis – is an increasingly common condition, often called “the silent disease”.
“Every thirty seconds someone in the EU suffers a fracture due to osteoporosis. Fractures of this kind cannot be repaired properly using metal plates and screws because the bone is so brittle.”
The vision is to change the whole landscape of fracture surgery. Doctors of the future will have access to a complete toolbox when they treat bone trauma. Malkoch elaborates:
“I want future surgeons to be able to do what dentists can do today. They can tailor treatment of cavities using composite materials. I want to do the same in the body using innovative and non-invasive materials that are eventually broken down and disappear without trace.”
Text Nils Johan Tjärnlund
Translation Maxwell Arding
Photo Mads Lüchow