Project Grant 2017
Molecular structure of mucin domains and role of their interactions
Principal investigator:
Professor Gunnar C. Hansson
Co-investigators:
University of Gothenburg
Malin E. V. Johansson
Göran Karlsson
Gergely Katona
KTH Royal Institute of Technology
Hans Hebert
Institution:
University of Gothenburg
Grant in SEK:
SEK 29 million over five years
The mucus in our bodies is produced by the mucous surfaces, mainly in our intestines and lungs. The intestine has a surface area as large as a football field, the lung equals an area the size of a tennis court.
“Just a few years ago it was still believed that the mucus coating the mucous surfaces was like a simple carpet. Our research has shown the contrary – that it is a highly dynamic system. Sometimes it is more permeable, sometimes less,” explains Gunnar Hansson, Professor of Medical Biochemistry.
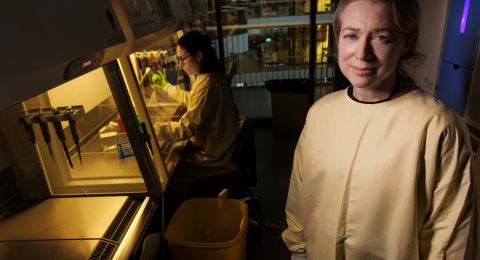
He has been researching on mucus for almost 30 years. Now he is heading a project involving researchers from the University of Gothenburg and KTH Royal Institute of Technology centering on mucus molecules themselves, known as mucins. They are large molecules with complicated structures: threads, balls and nets. They change shape and interact with each other, building up protection for the mucous surfaces so that it is not harmed by the acid in the digestive tract, by detritus or bacteria. Our intestines are home to billions of bacteria that are of great benefit, but that must not come into direct contact with the intestine. If they do so, the intestine may become inflamed.
Intestinal mucus impacted by diet – via bacteria
Mucus is constantly renewed by special mucus-producing cells, which are also capable of serving as “weapons”. If bacteria manage to penetrate the barrier, the cells can fire off a mucus ball to repel them. But mucus is more than just a protection – it also serves as food for the bacteria inhabiting the intestine. They don’t just eat mucus, however; they also feed on the same food that we eat. This means that our choice of diet seems to impact the mucus. Hansson and colleagues have made studies of mice showing that a typical western high-fat, low-fiber diet renders intestinal mucus more permeable. This increases the risk of bacteria penetrating it and causing inflammation. If mice are given a fiber supplement, their mucus becomes more resistant in just a few days. The researchers in Gothenburg believe the explanation to be that certain bacteria signal to the cells to make more viscous mucus, and that those bacteria specifically thrive on dietary fiber.
Mucus in close-up
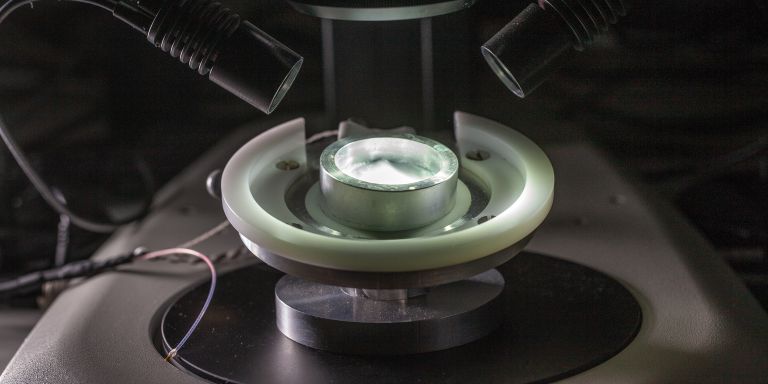
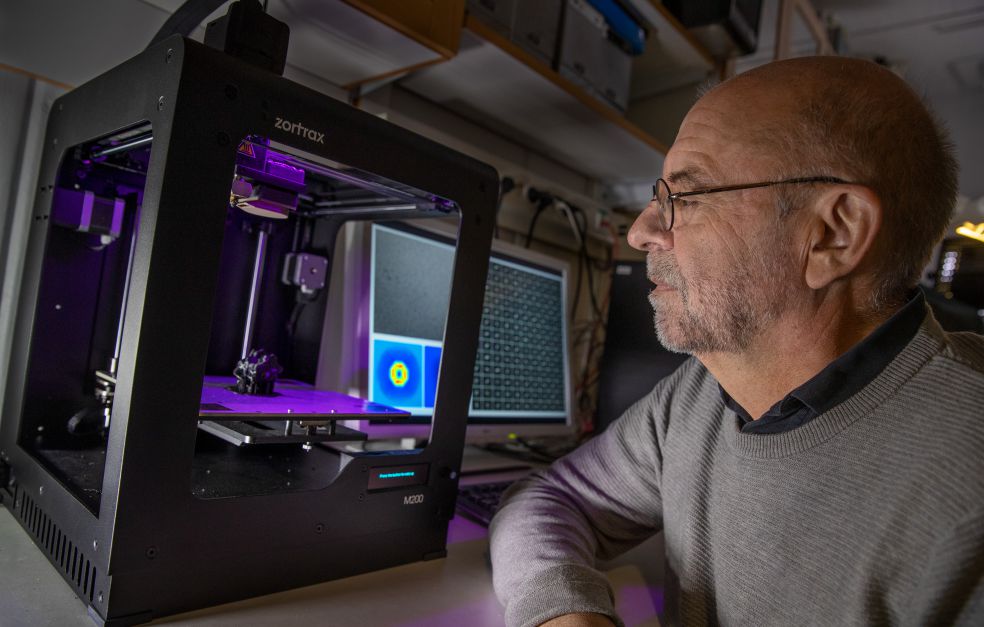
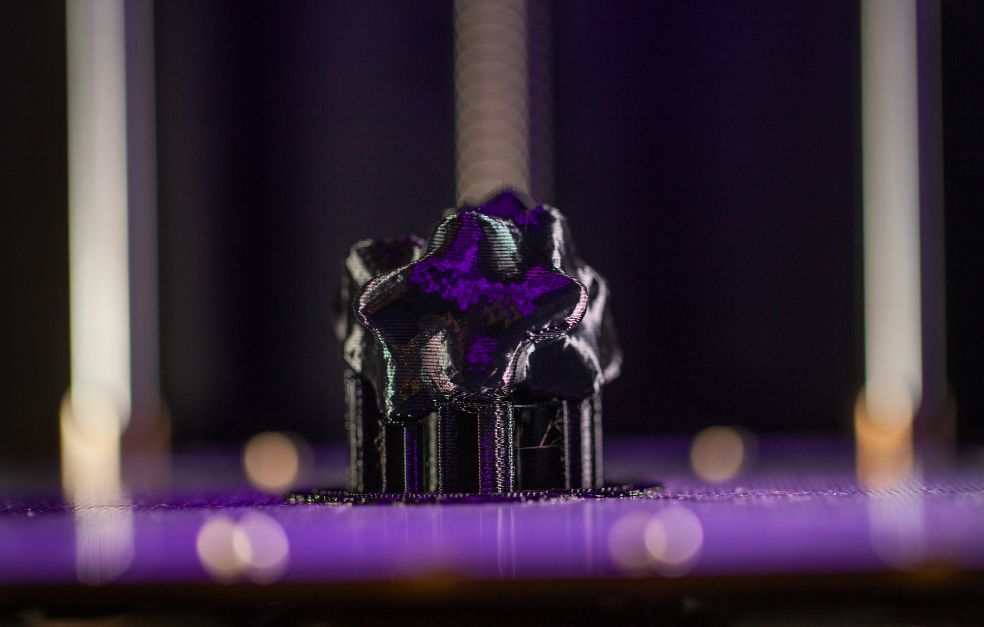
In the new project the researchers want to elucidate the structure of mucins and study how they join together to form mucus. Among other things, they are taking genes from the mucus-producing cells and using them to make various protein parts that make up the mucins. This delivers the complex mucin molecules in fragments that the researchers can study one piece at a time, as a step to understanding the big picture. Sometimes the researchers go even further and use models derived from electron microscope images of the mucins to print them out on a 3D printer.
“We could then see that the ends of one mucin packed in perfect pairs. That was what we had expected, and when we took a closer look, our ideas were confirmed,” Hansson explains.
New lung disease drugs
But the project is not targeting intestinal mucus alone, it also includes lung mucus. Here, the normal mucus does not cause problems. The problem is instead the thick, viscous mucus layer produced in a number of serious diseases such as cystic fibrosis, COPD and chronic bronchitis.
Under the electron microscope, the researchers have seen that the lung glands expel mucins in long fibrous bundles. The bundles sweep over the surface as moved by cilia, which are small hairs on the cell surface, picking up waste matter on the way.
The mucus bundles are in contact with the cilia and kept in place by other surface anchored mucus molecules so that they do not detach or move in the wrong direction. But in people with lung disease the mucus bundles remain immobile. As yet, the researchers do not know why.
“If we can understand the overall process, and how the molecules bind to each other, we might be able to find ways of preventing them from connecting and releasing the mucus bundles,” says Hansson.
This would be a completely new way of combating these diseases, and offers scope to develop new drugs.
“No new drugs for treatment of respiratory diseases have been developed over the past 30 years,” Hansson points out.
The opposite approach – to make the mucus bind together more – is also possible, but more difficult. When scientists manage to do that, the door will open for new therapies for inflammatory bowel diseases. But that is a matter for the future.
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström