
Göran Karlsson
Dr in Medical Science
Wallenberg Academy Fellow 2015
Institution:
Lund University
Research field:
Cancer stem cells in chronic myeloid leukemia

Wallenberg Academy Fellow 2015
Institution:
Lund University
Research field:
Cancer stem cells in chronic myeloid leukemia
The early 2000s saw the arrival of a revolutionary new drug for CML sufferers. All forms of cancer involve uncontrolled cell division. In this case the result is an overproduction of blood cells. Blood cells are produced by blood stem cells in the bone marrow. CML makes a genetic change in those cells, causing them to manufacture a rogue protein that drives rapid cell division. The medicine blocks the protein; cell division is arrested and the sufferer can live out a normal life.
But hidden in the bone marrow are a small number of pathogenic cells resistant to the treatment. They lie in wait, ready to restart the whole process. They are called cancer stem cells, and act as cancer progenitors. Their survival does not appear to depend on the rogue protein.
“Cancer stem cells are so few and so similar to normal blood stem cells that it has been impossible to find them. So we haven’t been able to analyze what makes them unique either. Only when we know that will we be able to fight them,” says Karlsson, who is a Wallenberg Academy Fellow and researcher at Lund University.
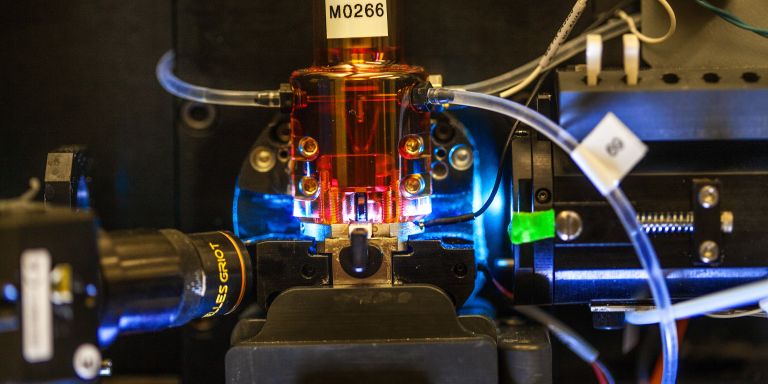
Karlsson and his colleagues have developed a new analytical method of finding the cells. They take a bone marrow sample from a CML patient who is undergoing treatment, and first remove all blood stem cells from the sample. Those cells are then placed one by one on a chip that reveals exactly which molecules each cell is itself producing. This results in a molecular “fingerprint” that differs as between leukemic stem cells and healthy blood stem cells.
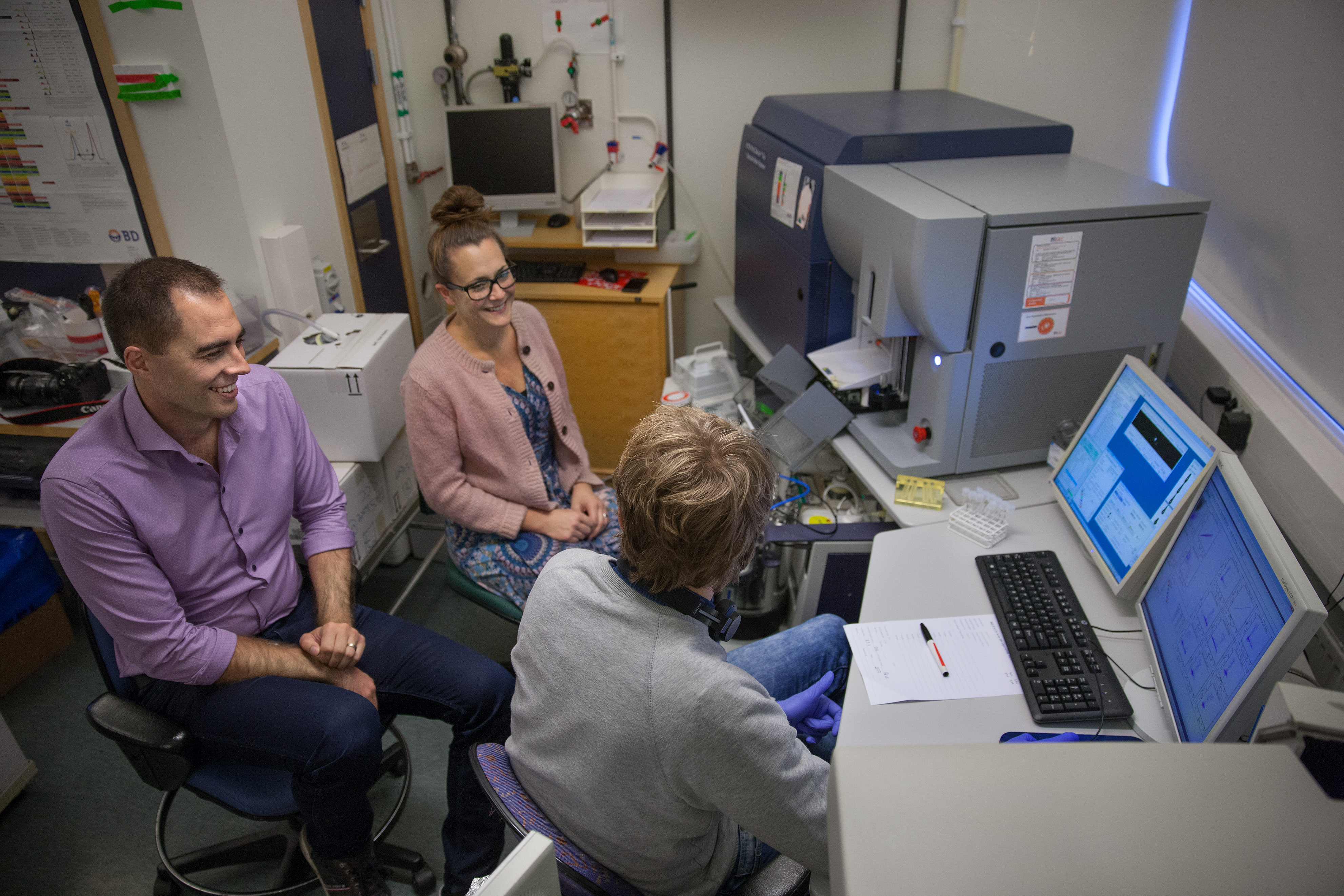
“We might find three of four leukemic stem cells in a patient sample containing hundreds of blood stem cells. Sometimes we don’t find any at all – so there are very few of them, but they are extremely relevant,” Karlsson says.
If the researchers can figure out the unique features of leukemic stem cells, they will have made great strides toward a treatment capable of eradicating them – and thereby the disease itself – from the body.
“Working as a researcher is a pretty tough job, with many setbacks. This makes success all the more important. As a Wallenberg Academy Fellow you feel a little bit special – someone believes in you. We need that kind of motivation. And the grant represents a lot of money for research. It gives the team the freedom to think big and be more creative.”
Karlsson believes that cancer stem cells resist treatment because of “epigenetic” changes. Each cell contains a full set of our genes, but the majority of genes in each cell are “silent”. Epigenetic factors controls which genes in a cell are expressed, i.e. activated, and which remain unused. Activated genes cause the cell to manufacture proteins. The type of proteins produced determines the type of cell that results. This will often also determine whether the cell becomes diseased or healthy.
Examples of epigenetics are that the DNA chain can be folded in different ways, thereby exposing different genes, or that molecules can be connected to the chain, and function as tiny start and stop signals for decoding.
If epigenetic differences can be found in cancer stem cells, it may be possible to develop drugs targeting them. This approach has been successful with a number of other diseases.
“When we have shown that our analytical method works, we will be able to extend it to other types of leukemia, and to other areas where the aim is to identify and isolate abnormal cells. After all, cancer stem cells appear to be present in virtually all forms of cancer, and this exposes patients to the risk of relapse. We should be able to use new drugs to prevent this – and now we no longer need to work in the dark.”

Karlsson’s goal was never to become a researcher. He simply did what he most enjoyed. He liked biology and chemistry at school, so he began studying biomedicine. When it was time for his master’s thesis, he decided to write about gene therapy and stem cells. He became increasingly interested in the nature of research – the ideas behind it and how it is organized. But when he was offered a doctoral position in the team where he worked, he did not even know what it was. Now he is a stem cell biologist, and he turned to the study of cancer because CML is a disease that is well-suited for testing theories and methods.
“Perhaps I should have realized earlier that research was my thing, but it only dawned on me when I had really got into it. Now my life is research, and I think about our projects and the challenges we face all the time. I never view anything as insoluble; I simply expect to find an answer in the end. When we discuss what we do here at the lab, I usually say we cure cancer. It might sound a bit naïve, but I really mean it. You have to believe it; otherwise it wouldn’t be as much fun going to work every day.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström