Project Grant 2014
Hitting cancer on target – Novel strategies for optimizing drug target engagement for improved brest cancer therapies
Principal investigator:
Jonas Bergh, Professor of Oncology
Co-investigators:
Sir David Lane
Yihai Cao
Pär Nordlund
Institution:
Karolinska Institutet
Grant in SEK:
SEK 39.6 million over five years
“The long-term goal of our research is to identify more reliable methods for optimizing the choice, use and dosages of drugs used to treat cancer. We will begin with breast cancer,” says Jonas Bergh, Professor of oncology at Karolinska Institutet.
Breast cancer is one of the commonest forms of cancer in Sweden. Each year just over 9,000 breast cancer tumors are found in women, and 50 in men. The survival rate used to be about 50 percent, but nowadays the prognosis is better: some 90 percent of patients are still alive five years after diagnosis; after ten years the survival rate is about 80 percent.
The options available for treating breast cancer are surgery, chemotherapy, hormones, radiotherapy and immunotherapy. But as yet there are very few methods of studying the effects of various drugs at molecular and cellular level.
“At present we choose drugs for cancer treatment on the basis of studies of a large number of patients in which drug A is compared with drug B to find out their average effects. The problem with this approach is the huge variations in the way that different individuals respond to a certain drug. This means that many people are given drugs they do not need, and others are given the wrong drugs.”
Several reasons for variation
The wide variations in patient response may occur because drugs are transported and absorbed by the body in different ways in different patients. Another reason may be that tumors react differently when treated with drugs. In some patients, cancer cells also become resistant to certain drugs. This may be because the proteins to which the drugs normally bind mutate, assuming a different three-dimensional structure, and therefore no longer work as a target for the drug.

“This is why it is important to learn more about the effect of various drugs on individual patients and tumors, as well as the molecular biological and genetic conditions needed so that different drugs can bind to cancer cells.”
The researchers will be using a number of model systems: cell lines, animal models, and eventually patients. The basis of their approach is to combine studies of how a tumor reacts to a given drug, and studies of the molecular biology and genetic conditions in the tumor.
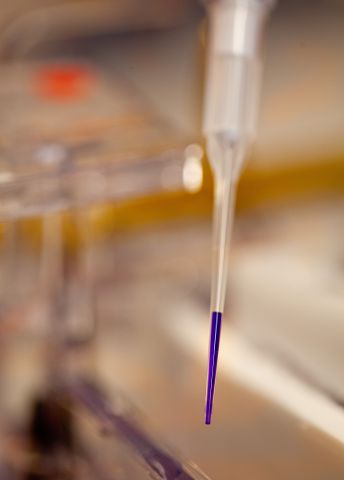
In practical terms, the project involves making a needle-stick in the tumor before and after a drug is administered to see how well the drug binds to the target proteins in the tumor. The researchers are also performing highly detailed molecular biological characterization of the tumor, studying the entire genome – the DNA – and also the genetic conditions and changes occurring.
Groundbreaking technology
Central to the project is a new groundbreaking technique called CETSA.
“The technique is extremely elegant, and enables us to monitor exactly how different drugs bind to their targets in the cell. Drugs for the treatment of breast cancer in current use, and those being developed will be systematically tested using CETSA to characterize the engagement of the drug substances with their targets in the cancer cells.”
The project will also include studies of the processes regulating the formation of new blood vessels, known as “angiogenesis”, as well as the protein p53, sometimes called “the guardian of the genome”, since it activates several genes that promote cell death and suppresses mutated genes that give rise to tumor cells.
Challenges
Researchers in the project face a number of challenges. One is getting the CETSA technology to work on all relevant drugs. Another is to understand differences between drug-target protein binding and functional effect, since there may be resistance mechanisms preventing the tumor cell from dying even though the drug binds well.
“A third challenge is that it is not certain that what works in cell lines and in animal models will also work on patients. This is because human cells are extraordinarily complex, and there may be components involved preventing us from understanding the processes involved.”
Better treatment
Professor Bergh is also an oncologist (cancer doctor), specializing in translational research, i.e. research designed to shorten the route from laboratory discoveries to clinical practice. His long-term goal is more skilled and effective treatment, so that more patients experience alleviation of their symptoms, and more are also cured of their cancer.
“I think that our research offers great potential to make a real difference by identifying new forms of breast cancer therapy. Our findings may also be of use in the treatment of other types of cancer.”
Text Anders Esselin
Translation Maxwell Arding
Photo Magnus Bergström



