Project Grant 2016
Characterization of the antibody response against epitopes at the core of host-bacteria relationships: the protein-protein interaction interfaces
Principal investigator:
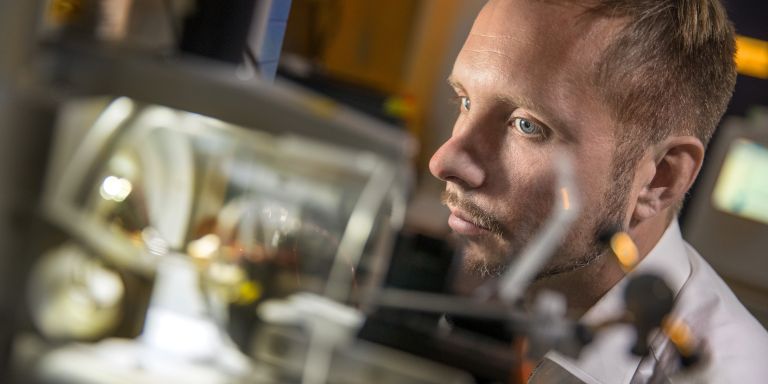
Johan Malmström, Professor of Infectious Medicine
Co-investigators:
Lund University
Lars Björck
Oonagh Shannon
Pontus Nordenfelt
The University of Zurich
Lars Malmström
Institution:
Lund University
Grant in SEK:
SEK 16.6 million over two years, with the possibility of a three-year extension
Every year some 700,000 people die from untreatable infections. They are infected by bacteria resistant to current drugs. The problem is mushrooming – in 30 years there may be 10 million fatalities a year unless we come to grips with the problem. Resistance must be slowed, but we also need to find new ways of fighting disease-causing bacteria.
Many research teams around the world are working on precisely this problem. One of them is based at Lund University. A new project, funded by the Knut and Alice Wallenberg Foundation, sees researchers at Lund working with their colleagues in Zurich to study how the human body’s own antibodies defend us against bacteria. Their ultimate goal is to figure out how to make antibodies even better at their job.
Ideas about viruses translated to bacteria
The main task of antibodies is to mark bacteria, and summon the rest of the body’s defenses. Antibodies bind to proteins that are part of the infected organism, or are attached to it. Scientists already know quite a lot about this interaction between antibodies and surface proteins – but mainly as regards viruses. Bacteria are more complicated, and much less researched.
“So we are borrowing ideas from the virus field and translating them to bacteria with the help of new technology. And time is running out. The growing resistance to antibiotics is really worrying,” comments Johan Malmström.
He works at the Division of Infection Medicine at Lund University, and is heading the project on the interaction interface between antibodies and bacteria.
Mild illness or death?
The team in Lund and Zurich is studying “Group A” streptococci, bacteria that sometimes cause mild skin infections, sometimes deadly sepsis. That some people become seriously ill and others do not, has to do with the efficiency of their antibodies.
“Large numbers of proteins are attached to the surface of bacteria. Our earlier research has shown that they protrude from the surface like a forest. Huge numbers of antibodies bind to each tree in a very structured way. It is infinitely more complex than we first thought, and it was this realization that laid the foundation for the project.”
There may be up to 10 billion antibodies in a human body. A number of them bind to Group A streptococci, but each antibody type can only bind in a specific place. In some places there is little room and it is difficult to bind. And the ability of different antibody types to bind varies. So the most effective antibodies seem to be those that fit in somewhere where there is enough space and that also bind well. The aim is to find them, so they can eventually be used to develop new vaccines or drugs.
Mapping and testing antibodies
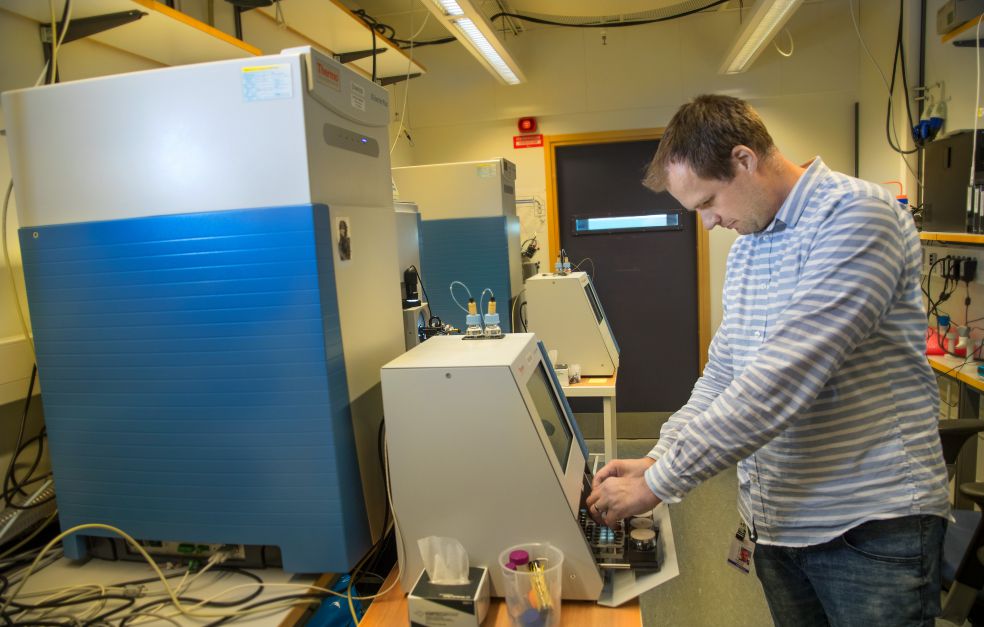
The first stage is for the researchers to focus on a single protein from the surface of the streptococci. Their aim is to find the antibodies that bind best to it, map their structure and exactly how they bind. To do this, the team is developing new analytical methods based on mass spectrometry, a technique for sorting proteins according to their mass. Advanced bioinformatics will also be needed. Mathematical methods and computer models make it possible to analyze huge quantities of information.
“There’s a monstrous amount of data,” Malmström says.
The mapped antibodies will be tested both in cells and in mice. The mice will either be vaccinated so they start to produce their own antibodies of the type the team wants to study, or they will be injected with “ready-made” antibodies.
The final step will be for the researchers to incorporate the new knowledge and new techniques, and test them on other proteins and groups of bacteria.
New methods must be scalable
“We are aiming high, and will be doing difficult things that you can’t look up in a book – things that will demand completely new techniques. After the first protein, there are at least another two hundred surface proteins that would be of interest. After that there are another forty or more disease-causing bacteria… We won’t be able to study them all, of course. But one of the aims of the project is to develop new methods for large-scale study of the interaction between various bacteria and antibodies.”
In the future it may be possible to use advanced computer models to work out the shape of antibodies that would maximize their ability to bind, and to tailor them for that purpose. More and more important research is being done on computers. Malmström comments:
“But computer-based research alone is not a good thing. Experiments are also necessary. That’s why I am so glad to have gathered such a broad team of researchers. I think the Foundation’s approach is absolutely right – supporting research done by teams that are much larger than those normally found in a single lab.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström