
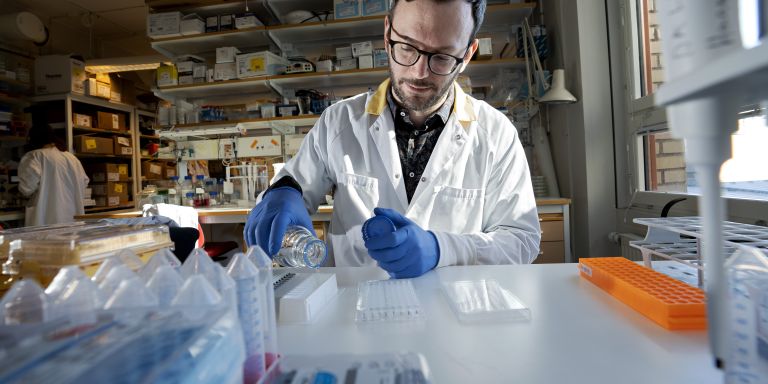
Davide Angeletti
PhD, Immunology
Wallenberg Academy Fellow 2021
Institution:
University of Gothenburg
Research field:
Antibody and B cell responses to influenza virus, influenza vaccinations

Wallenberg Academy Fellow 2021
Institution:
University of Gothenburg
Research field:
Antibody and B cell responses to influenza virus, influenza vaccinations
A virus infection, or a shot to protect against one, triggers a reaction in B cells in the immune system. They produce antibodies, and some of them, being able to remember the attacker, are quickly activated if the same virus shows up again.
But antibodies do not target the whole virus, only certain proteins on its surface. In the case of influenza, B cells primarily target a protein called hemagglutinin. Hemagglutinin resembles a miniature mushroom, on which parts of the cap often change shape due to mutations in the RNA of the virus, whereas the stem is more stable. Unfortunately, it is the cap that the antibodies target.
“Although the ‘stem’ of the protein remains unchanged to a far greater degree between different influenza viruses – including seasonal and pandemic variants – the immune system devotes the vast majority of its response to the ‘cap.’ We want to find out why this is,” says Angeletti, researching at the University of Gothenburg Department of Microbiology and Immunology.
The mutable protein means that a new seasonal influenza vaccine must be produced each year, adapted to cope with new virus variants. This requires a considerable amount of guesswork in good time, since the virus proteins have to be cultured in hen’s eggs. Angeletti explains that in the northern hemisphere, a decision on the composition of the vaccine for the autumn/winter season is made as early as April or May. The decision is based on the virus strains circulating in the southern hemisphere at that time combined with forecasting.
“It often works quite well, but sometimes not at all. And sometimes the protein mutates slightly while it is being cultured in the eggs. It’s not yet clear how such small differences can have such a big impact. In experimental animals, the influenza virus requires between twelve and fifteen mutations to avoid being recognized by the immune system, but in humans it only needs one,” Angeletti says.
New research has also shown that the B cells that can be activated by vaccination and produce antibodies against the vaccine virus, only survive in the body for about one year.
Angeletti’s research involves exploring the characteristics of B cells and trying to induce them to target a more stable part of the virus and increase their lifespan. This may form the basis for better vaccines with longer-lasting efficacy. His research team is using a number of technologies. One of them is flow cytometry, in which cells suspended in solution pass one by one through a laser beam where the light is scattered differently depending on the cell’s shape and characteristics. Another technology is single-cell analysis, in which the RNA or protein content of individual cells is analyzed in detail.
The researchers also modify mice genetically so they produce B cells that make antibodies targeting the lower rather than the upper part of the hemagglutinin.
“Using animal models enables us to keep close tabs on what comes in, and what happens during an infection. But it’s difficult to create models that are good enough. The situation in the human body is so complex. An adult may have encountered the influenza virus between ten and thirty times. How are we to replicate that situation? The models do give us some clues though.”
The dream is a vaccine against all influenza viruses that lasts a lifetime. But more realistic might be one that protects against all strains for five or ten years.
Angeletti is also comparing B cells in the lungs and upper respiratory tract to see how they differ. And he is studying another influenza protein – neuraminidase. This protein is not used in vaccines because it has been difficult to synthesize, and there have been no good, standardized methods to measure the activity of antibodies against it. The researchers now want to ascertain which parts of neuraminidase would make the best targets for future vaccines.
Angeletti grew up in Italy. He liked science and math in school, and originally planned to become an engineer. But he decided that would be too boring. Then he considered medicine – but realized he was not keen on blood. So he chose biology instead.
“I wasn’t impressed during the first few years. But I thought I might as well finish what I’d started, preferably abroad. I applied to join a number of masters programs before deciding on Karolinska Institutet. That was when things got interesting.”
He remained in Stockholm, receiving his PhD for a thesis on antibodies and malaria. He then took up a postdoctoral position in the U.S. at a laboratory using animal models to study influenza.
“It was half virology and half immunology. I started to appreciate the balance between the immune system and the virus itself – I was fascinated by the way one is constantly trying to adapt, while the other is trying to escape.”
In 2018 Angeletti returned to Sweden with his wife, who is also a researcher. They thought the work–life balance was better here, and the University of Gothenburg could offer high-quality research into the immune system in the respiratory tract.
“Although the Covid pandemic did result in an explosion of new knowledge, there is still much we don’t know. Until just a few years ago B cell immunologists were using very simple models. Now we have methods that create the potential for loads of new discoveries, which I think is definitely the most fun thing about science.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Johan Wingborg