Project Grant 2016
Characterization, Surveillance and Targeting of Cancer Stem Cells
Principal investigator:
Sten Eirik Waelgaard Jacobsen, Professor of Stem Cell Biology
Co-investigators:
Yenan Bryceson
Eva Hellström-Lindberg
Seishi Ogawa
Petter Woll
Institution:
Karolinska Institutet
Grant in SEK:
SEK 45.25 million over five years
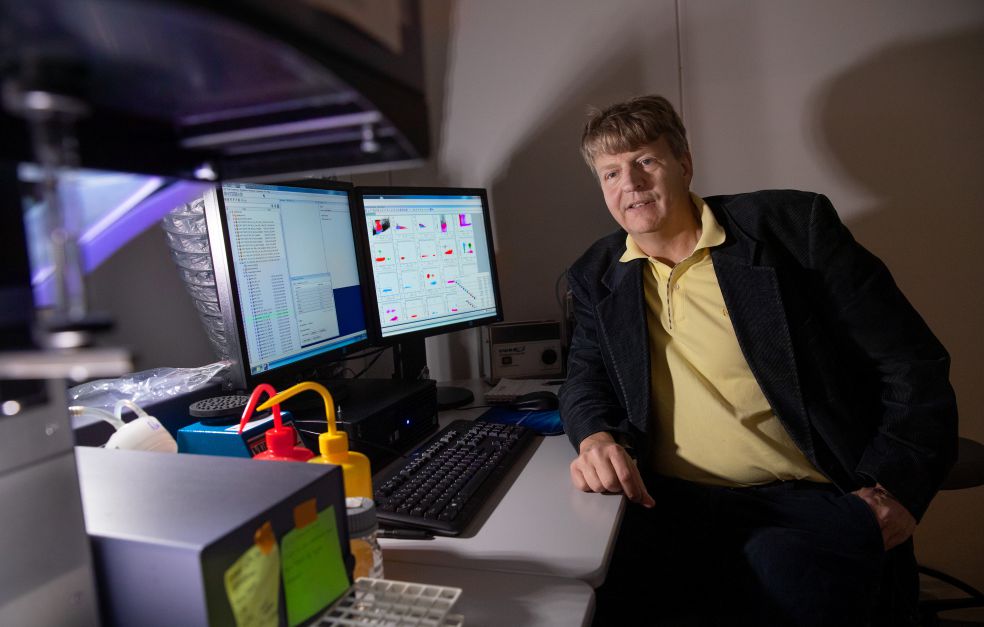
“This sort of instrument is essential to our work,” says Sten Eirik Waelgaard Jacobsen, pointing to an instrument called a flow cytometer in his laboratory at Biomedicum in Solna, north of Stockholm.
He is Professor of Stem Cell Biology at Karolinska Institutet, and has researched a great deal into how stem cells in the blood system form blood cells.
“Stem cells are essential to normal blood formation. An adult human produces millions of blood cells every second. Stem cells are the only cells that can renew themselves, and therefore the only cells that can produce blood cells of all types over a long life.”
With funding from Knut and Alice Wallenberg Foundation, Jacobsen is heading an interdisciplinary project involving five research teams. Their work centers on a cancer stem cell that has been found to play a key role in MDS – myelodysplastic syndrome – a form of blood cancer. These stem cells both trigger the cancer and are needed to maintain it.
“Cancer really is extremely difficult to cure. Dramatic improvements can be achieved with chemotherapy and other treatments, but unfortunately cancer returns in many patients. There are ample data showing that these stem cells are a key reason that therapies for MDS tend to be ineffective.”
MDS is most common among people over the age of 60, and often develops into more aggressive forms of leukemia. No one is cured without a bone marrow transplant, or a stem cell transplant as it is also known. But the high age of patients means that few of them are able to receive a transplant. Jacobsen elaborates:
“We have recently managed to identify the cancer stem cells in MDS more accurately, and we now hope to be able to monitor them in the patient so we can study whether or not different therapies successfully target these cells. We also want to study the cells in molecular and genetic terms, so we can try to identify targets for new and more effective therapies aimed specifically at these cancer stem cells.”
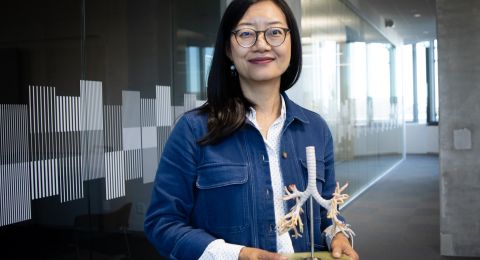
A clinical dimension
A cornerstone of the project is collaboration with the clinic at Karolinska University Hospital in Huddinge, south of Stockholm, where patients diagnosed with MDS are treated. The clinical research under the project is headed by Professor Eva Hellström-Lindberg, who has built up considerable knowledge of MDS, together with an extensive biobank of bone marrow from MDS patients. This is a huge asset to the project.
“For instance, we have an interesting study in which we have examined MDS stem cells in patients who have received bone marrow transplants. Two-thirds of them are actually cured. But one-third suffer a relapse, which may occur as long as ten years after the patient appeared to be free from cancer,” says Jacobsen.
Bone marrow samples are routinely taken from transplant recipients at the clinic to see whether traces of the tumor remain.
“We have examined bone marrow from patients who later suffered a relapse. In almost all cases we have found these cancer stem cells up to two years before relapse. When patients relapse it is essential to begin treatment as soon as possible. We hope to find tools for better treatment and prevention of relapse after bone marrow transplants.”
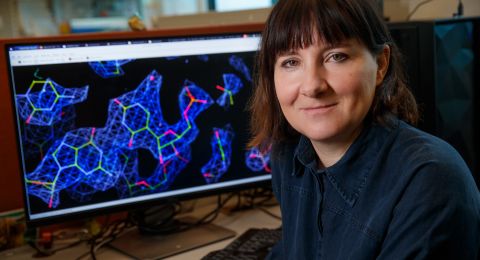
The researchers compare with normal stem cells, so they can understand what has gone wrong in the cancer stem cells. And therein lies the key to potential new therapies.
Multiple labs
“Our team is a dynamic one. To make progress on the really major issues in medical research, you have to gather skills and expertise of different kinds,” Jacobsen explains.
Most project work is being conducted at the Neo research center in Huddinge, and also in Japan. A leading cancer geneticist has been recruited to the project, as a visiting professor at Karolinska Institutet, Professor Seishi Ogawa from Kyoto University.
“His work is essential if we are to understand what is dysregulated in the cancer stem cells. Petter Woll and I are both interested in stem cell biology in MDS, and Yenan Bryceson is researching on immunotherapy – using the immune system to attack stem cells in MDS. Research in immunotherapy received the Nobel Prize in Medicine in 2018.”
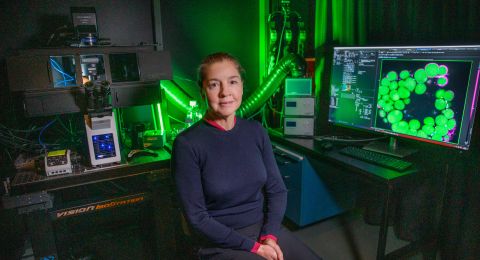
Using flow cytometry, the researchers can analyze 100,000 cells a second.
“The flow cytometer can not only identify the rare cancer stem cells; it can also sort them out from other cells. Importantly, the cells are still alive, which means we can then characterize them in every conceivable way, right down to individual cell level.”
The concept of cancer stem cells is debated. It is unclear whether and exactly how it works in each form of cancer, but the basic principles are likely very similar, as Jacobsen points out:
“I think that important discoveries in this project may have implications for how cancer stem cells in other cancer systems are viewed.”
Text Susanne Rosén
Translation Maxwell Arding
Photo Magnus Bergström