
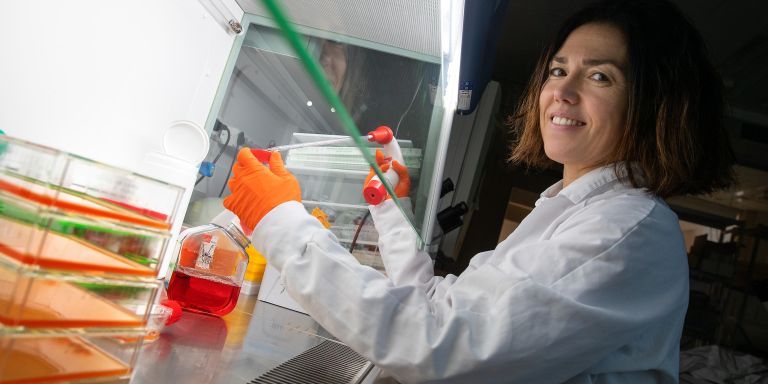
Itziar Martinez Gonzalez
PhD, Immunology
Wallenberg Academy Fellow 2019
Institution:
Karolinska Institutet
Research field:
ILC2 immune cells and their links to allergy

Wallenberg Academy Fellow 2019
Institution:
Karolinska Institutet
Research field:
ILC2 immune cells and their links to allergy
When she was growing up in Spain Martinez Gonzalez wanted to be a private detective. She started reading medical thrillers in her teens, and her dream shifted a little. But she still wanted to solve complicated problems.
“When you find the answer to something you were wondering about – it’s a great feeling. There are a lot of doctors in my family. I’m sure it was one of the reasons I started studying biology and became interested in the immune system.”
Her research centers on links between asthma and atopic dermatitis (flexural eczema), which affects about one in five infants in Sweden. It is known that those with the most pronounced symptoms run the risk of developing asthma, but the reason for this is not known.
“The reason might well be that these children run a genetically elevated risk of developing allergies of various kinds. But the correlation between eczema and asthma is so strong that it is worth asking whether one somehow causes the other.”
The immune system can be divided into two parts: the innate system and the adaptive (or specific) one. The innate immune system is the first line of defense, with cells that rapidly but non-specifically react to infectious agents, destroy alien organisms and muster other immune cells. The adaptive system is activated more slowly, but can adapt to substances and infections by forming antibodies so the body can defend itself more quickly next time.
Allergies occur when the immune system overreacts. Substances causing these reactions are called allergens. Examples include food, pollen or chemicals. Allergic reactions are usually explained by reference to an “immunological memory”, which researchers to date have linked to the adaptive immune system. But Martinez Gonzalez’ hypothesis is that the innate immune system is also involved.
Her work centers on “ILC2 cells” (type 2 innate lymphoid cells). These are lymphocytes – immune cells present in our immune system from birth. They react quickly and non-specifically, protecting us from parasites. They also play a key role in wound healing, for example. They are mainly found in superficial tissues, such the mucosa and skin and in lung tissue.
During her time as a postdoc in Canada Martinez Gonzalez studied mice with allergic inflammation to see how their ILC2 cells reacted when exposed to various allergens. To her surprise, she discovered that the cells remained long after the onset of the inflammation. This did not accord with the role usually ascribed to them. They should have been active at first and then disappeared. Six months after the first inflammation, she exposed the mice to an allergen. She found that they became sicker than other mice that had not experienced an inflammation with activated ILC2 cells. ILC2, which had been thought not to possess any “memory capacity”, reacted more quickly and vigorously if they had been active before. The researchers began to refer to the cell type as “memory ILC2”, and the hypothesis is that they may be one of the causes of asthma in patients with eczema.
“This reaction is not specific to a given antigen; anything that damages the epithelium and triggers an immune response also triggers the memory ILC2 cells. This redefines what we have previously called immunological memory.”
Martinez Gonzalez is now studying reactions in mice that are exposed to different allergens, and identifying the places in the body where activated ILC2 cells are present. The cells can circulate in the blood, and appear to gather in the lungs if the antigen is administered to the mice via the nose. This supports the hypothesis that the cells can trigger asthma.
She will also be working with genetically modified mice that do not produce ILC2 cells, so she can rule out the possibility that a completely different mechanism or cell type is responsible for what she has observed. In the future she also wants to conduct studies to analyze more cell types, and samples from asthma sufferers.
“If we can figure out which molecules or receptors are important for memory regulation, we may be able to find ways to block some of them, or prevent them from migrating to the lungs. We don’t want to block all of them, because they’re needed in the body, but we might be able to block specifically the memory ones to achieve a milder response.”
Martinez Gonzalez expects to be working on ILC2 cells for a long time to come. She believes the field will be of growing importance.
“Being a Wallenberg Academy Fellow means receiving very important economic support, but I also feel that I have become part of a research family that takes care of me. This is particularly valuable for me as a foreigner.”
“When I was working as a postdoc in Vancouver, I enjoyed backpacking – the mountains are beautiful there. An academic career is like walking in the mountains. You have to be motivated, because it requires an enormous effort – you have to remain focused and be persistent. Some days to need to step back and you can’t let disappointment get to you. But sometimes it’s extremely exciting. You can reach the top of the mountain – one small step at a time.
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström