Project Grants 2011
Bacterial modulation of early clearing responses and its effect on infectious disease outcome (BERIDO)
Principal investigator:
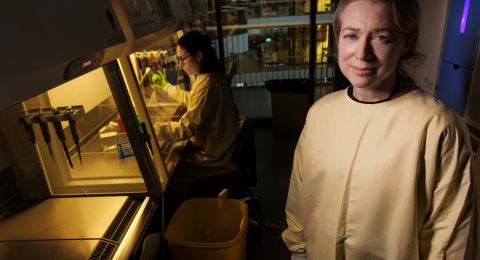
Birgitta Henriques Normark, professor of clinical microbiology specializing in clinical bacteriology
Co-investigators:
Anna Norrby-Teglund
Juha Kere
Adnane Achour
Fredric Carlsson
Staffan Normark
Institution:
Karolinska Institutet
Grant in SEK:
25.8 million over five years
Birgitta Henriques-Normark directs a research project that seeks to enhance our knowledge of what causes infectious diseases and what the connections look like between bacteria, humans (the hosts), and immune cells.
“Pneumococci, which can cause lower airway infections like pneumonia but also blood poisoning and meningitis, are also found in the noses of many healthy children and some adults. We want to know why they sometimes cause fatal diseases.”
It’s becoming more and more urgent to answer this question, as the development of resistance to antibiotics can make it difficult to treat diseases with today’s antibiotics.
In Sweden there are some 1,400 cases of severe pneumococcal infections annually, but it’s above all in developing countries that these infections are claiming lives. One solution is to create a vaccine that protects everybody against all variants of pneumococcus. Today’s vaccine only protects against a limited number that cause the most severe infections in the US. Another possibility is to find new antibiotics.
Different bacterial strains
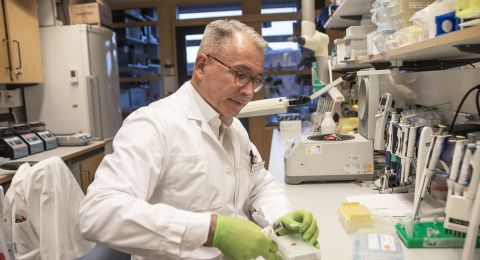
The research project is a so-called translational project, which means that the researchers are studying the whole chain – from molecule to patient.
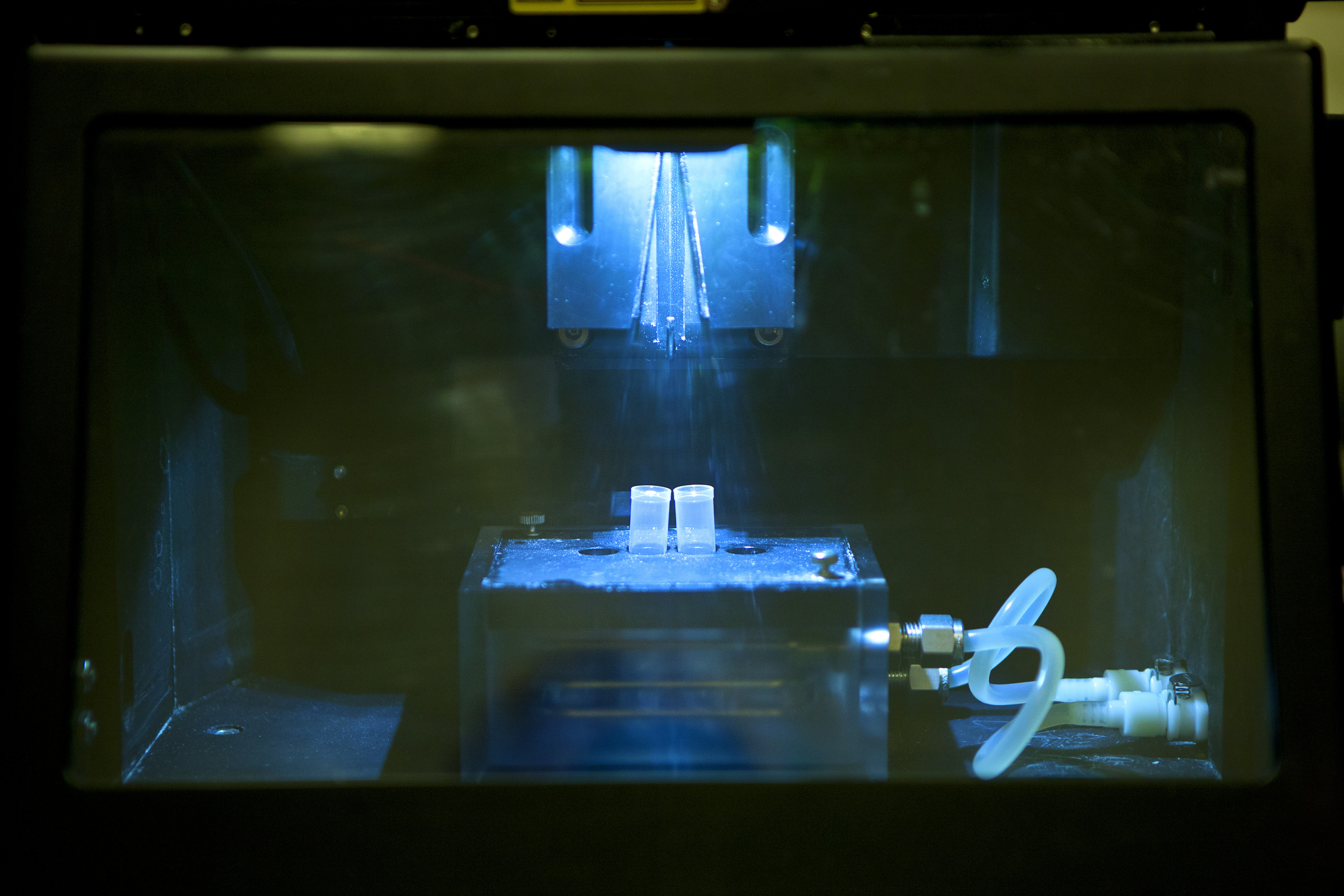
“We are looking at the interplay between the bacterium, the host (humans), and immune cells. We have bacterial strains from patients that we examine both in vitro (in test tubes) and in vivo (in living organisms) to try to understand what causes disease. These bacterial strains comprise both those that lead to severe diseases and those that exist in humans without causing disease.”
“Using various molecular techniques, we characterize the strains to see, among other things, what significance their genes have in the development of disease. We can then go on to create mutations by removing genes to see what role they play in how bacteria can bind to cells in the mucous lining, for example, or how they interact with immune cells,” explains Birgitta Henriques-Normark, professor of clinical microbiology, Karolinska Institutet.
“Bacterial hair” of importance
But she is also trying to figure out what makes some people extra susceptible to infections. In the lab they are working with models for lung tissue.
Immune cells and their helpers defuse the bacteria. If they fail, the bacteria spread further and begin to destroy the tissue.
“We believe that what happens early in the course of an infection is important and that the congenital immune defense plays a significant role. Early elimination of bacteria in the course of an infection is key.”
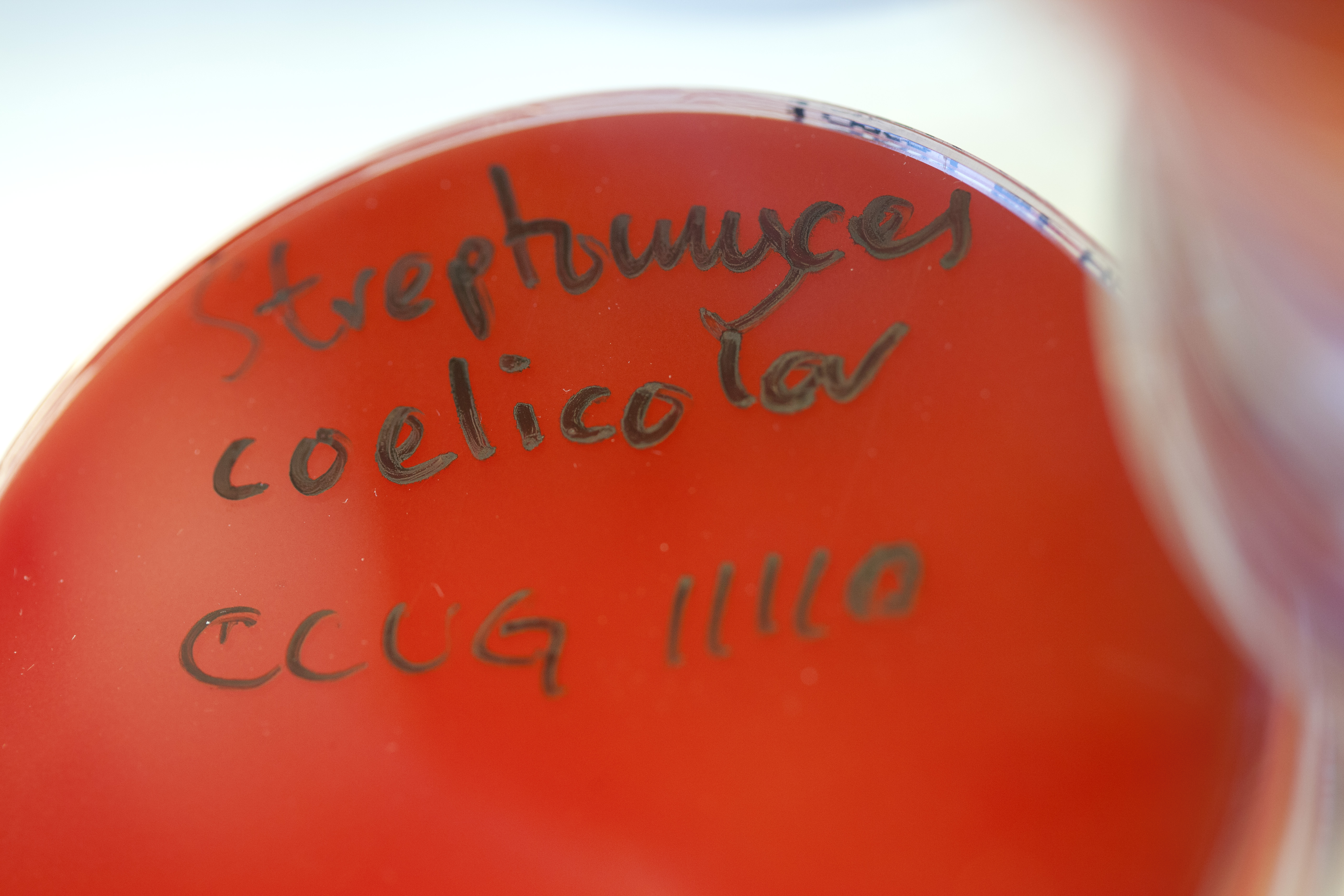
Among other things, they are looking at a complex of proteins that are called inflammasomes and play a role in how the built-in immune defense is activated. The differences in the appearance of the capsule surrounding the pneumococcal bacteria are also of great interest.
“There are at least 97 different capsule types. Some cause disease and others don’t. But other factors also make a difference. Some have a pilus, a hair-like structure that helps the bacteria to fasten to the mucous linings of the body. We have a few candidate genes for vaccines on the bacterial side but also a number of ideas regarding the receptivity of certain individuals,” says Birgitta Henriques-Normark.
Certain population groups more susceptible
Birgitta Henriques-Normark’s research team was the first to discover pili on pneumococci. They also found that several genes in a so called “pathogenicity islet” play a role in how the pilus is formed.
“Some pneumococci have pili and others don’t. The pilus seems to play a role in how pneumococci spread around the world.”
The researchers also know that certain population groups, such as indigenous populations, are more susceptible than others to pneumococcal infections.
“Genes can be structured in different ways, and the structure of the host gene can make it more, or less, susceptible to the bacterium,” explains Birgitta Henriques-Normark.
More effective vaccine
In 2009 the pneumococcus vaccine was added to the general children’s vaccination program in Sweden, and Birgitta is following this up at the Swedish Institute for Communicable Disease Control.
“In Stockholm vaccinations started to be given in 2007. Children function as reservoirs for pneumococci. In Sweden roughly 40 percent of children attending day care centers have the bacteria in their noses without being ill, while in other countries this figure can be as high as 60 to 70 percent.”
The rationale behind the vaccination is to reduce morbidity, which could save many lives in developing countries.
“The vaccine provides protection against a limited number of pneumococci, depending on which capsule surrounds them, but it does protect against several of those that cause severe infections in the world.”
Birgitta Henriques-Normark hopes that it will be possible to develop a more general vaccine that can protect against all pneumococci that exist in society and cause disease.
Text Carina Dahlberg/KAW
Translation Donald S. MacQeen
Photo Magnus Bergström
Some example of infectious diseases
Childhood diseases, such as: German measles, measles, chicken pox, mumps
Blood poisoning (sepsis)
Borrelia infection
Shingles
Chlamydia infection
Gonorrhea
Hepatitis
Herpes
HIV
Heart valve infection (infective endocarditis)
Skin infections
Influenza
Pneumonia (pneumococci)
Malaria
MRSA (staphylococci)– “hospital disease” (noscomial infection)
Myobacterial infection
Plague
Polio
Rabies
Salmonella
Sarcoidos
Skeletal and joint infections
Smallpox
Urinary tract infections
Intestinal infections
TBE (tick-borne encephalitis)
Tuberculosis
TWAR (chlamydophila pneumoniae)
Winter vomiting disease