Project Grant 2015
Systems precision medicine platform to optimize therapies for cancer patients: acute myeloid leukemia (AML) and beyond
Principal investigator:
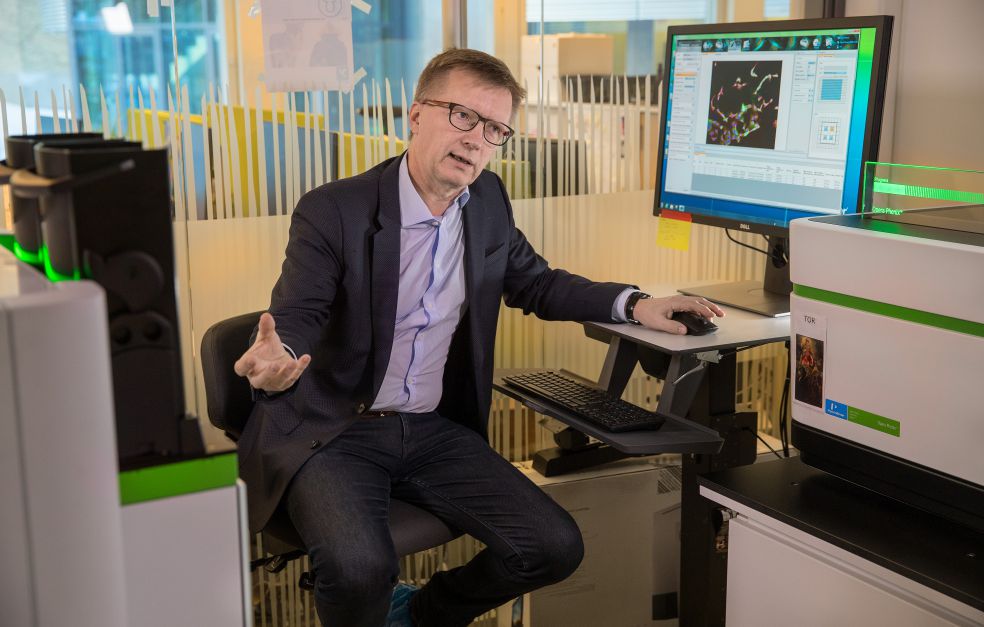
Olli Kallioniemi, Professor of Molecular Precision Medicine
Institution:
Karolinska Institutet
Grant in SEK:
SEK 46 million over five years
“Far too many of today’s drugs have been developed in line with the ‘one size fits all’ principle. We are examining how we can tailor therapies to individual cancer patients so they are safe and effective, using the right drugs at the right time,” Kallioniemi says.
The Knut and Alice Wallenberg Foundation has awarded him a grant, which his research team is using to build an infrastructure and research environment at the Science for Life Laboratory (SciLifeLab) in Solna, north of Stockholm. The goal is to gain a complete molecular picture of cancer cells. Hundreds of existing drugs are also being tested on cells from patients.
These methods can also be used to speed up the development of new, more targeted cancer drugs. Kallioniemi explains:
“Our research may also be of benefit in our collaboration with other research teams, and for pharmaceutical companies in selecting the most promising development projects.”
Testing hundreds of drugs
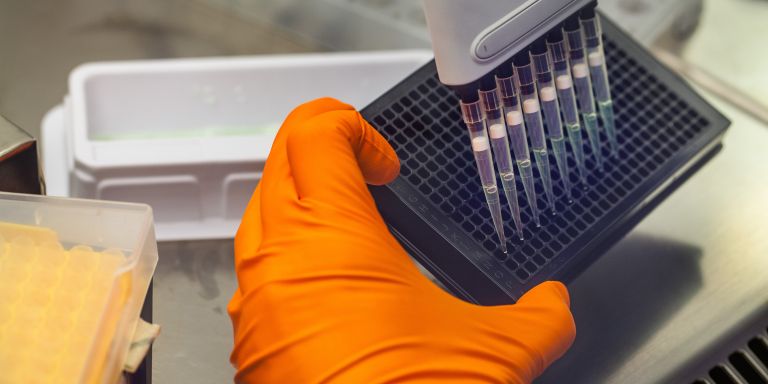
Kallioniemi shows a measuring instrument and a microscope, used for monitoring and imaging the way cells from patients react to 460 different cancer drugs. The project obtains cell samples from a biobank of blood and bone marrow samples from patients who have been treated for acute myeloid leukemia (AML).
“Later on we hope to receive patient samples direct from cancer clinics – we have the ethical permits to do so. Our aim is eventually to be able to give feedback to the clinics. But first we need to know that the system works, and that doctors can interpret the molecular information they receive.”
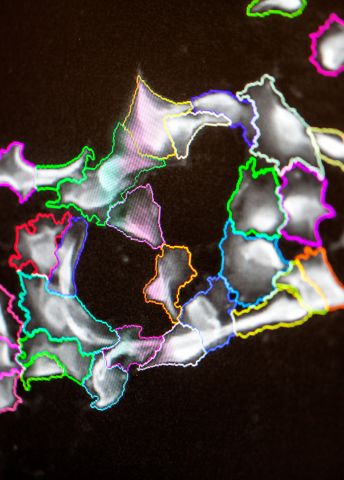
Kallioniemi explains that each patient sample is tested with different doses of each drug. He points to a computer display showing hundreds of small squares in different colors.
“We can study one cancer cell at a time, monitor it, and see how it responds to the drug over time. After three or four days we can gain an idea of how effective or ineffective the drug may be.”
In current cancer treatment it can take weeks or months before doctors know whether a drug is working on a patient. The methods that Kallioniemi’s team is developing are intended to enable the care team to understand what is happening in the patient’s cells, even while treatment is still in progress.
They have chosen to study leukemia – cancer of the bone marrow where blood is formed – because those cancer cells are easier to remove from a blood sample than from tumors in tissue. The ultimate aim is also to study solid tumors. The researchers have already begun to study cells from ovarian tumors.
Molecular profiling
The researchers are also conducting molecular profiling of cancer cells from patients, to understand why they behave as they do.
“We sequence cell DNA, and study aspects such as genes and proteins that are expressed. Our research would not be possible without the environment and tools available at SciLifeLab. The lab has world-class equipment – many of the instruments are accredited for clinical use.”
It is also possible to identify new applications for drugs that have already been approved by testing large numbers of drugs on a cancer cell. One discovery made by Kallioniemi’s team is that a certain type of relapsed leukemia can be cured using a drug intended for kidney cancer.
“The scope of the project gives us the freedom to test all drugs on cells from patients. But translating how these data can be used in the patient’s specific therapies is highly complex, and involves a number of medical, ethical, legal and regulatory issues. New treatments are normally introduced by way of clinical trials – trials whose design may be influenced by our findings.”
New regulations needed
In 2015 Kallioniemi moved from Helsinki University to take the next step in his work on precision medicine for cancer. He is both a professor at Karolinska Institutet and Director of SciLifeLab. The work of his research team at the Institute for Molecular Medicine Finland (FIMM), and the knowledge it has generated are gradually being transferred to Sweden.
Translational research, in which research takes place in close collaboration with the health care sector, has played a central role in Kallioniemi’s research career. He emphasizes that collaboration is the key to the systemic changes needed so that precision medicine for cancer can become a reality:
“Our work at SciLifeLab could benefit patients even now. But we are dealing with concepts that are not used in the health care sector or by the drug companies. We also need a solid framework within which our methods can be used. We need a new regulatory framework governing ethical, legal and financial dimensions.”
Summing up, Kallioniemi says cancer patients of the future will receive completely new, individualized therapies:
“And the current procedure for obtaining drug approval, requiring clinical studies on a thousand patients, will be history.”
Text Susanne Rosén
Translation Maxwell Arding
Photo Magnus Bergström