Project Grant 2013
Seeing organ function – patient specific image data
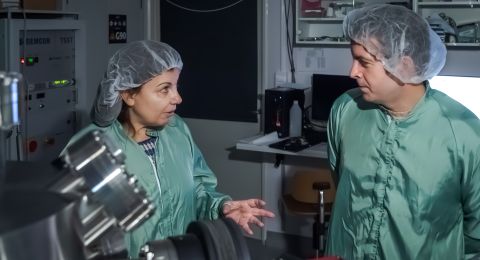
Principal investigator:
Anders Ynnerman, Professor of Scientific Visualization
Co-investigators:
Magnus Borga
Tino Ebbers
Maria Engström
Markus Heilig
Matts Karlsson
Hans Knutsson
Peter Lundberg
Claes Lundström
Anders Persson
Örjan Smedby
Karin Wårdell
Institution:
Linköping University
Grant:
SEK 24.5 million over five years
Tomography is the name for using radiation of various kinds to form images of the human body one layer at a time. Some of the most common methods are given acronyms: MRI, PET and CT (CAT-scan). Combined with advanced mathematical methods, they provide incredibly detailed images of our organs and tissues. But now it is time to move on from still images to film (3D time sequence of data).
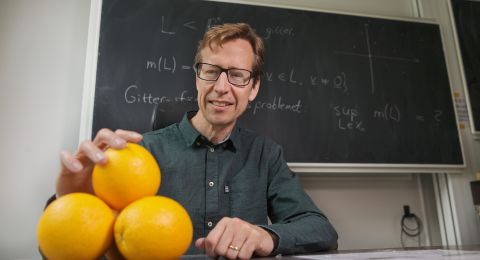
“We want to see what happens when the heart beats, or see how the different parts of the brain work,” says Anders Ynnerman, Professor of Scientific Visualization at Linköping University.
Functional data providing useful tools
In a project funded by the Knut and Alice Wallenberg Foundation, he and his team are working to develop current imaging technology. Functional data is data that describe bodily functions such as blood flow, movement, or diffusion – how water moves within and between tissues. With the help of these data it is possible both to study the processes and to make simulations.
The project involves experts in simulation technology, image analysis, flow simulations and brain simulations, radiologists, cardiologists and a medical co-coordinator. Professor Ynnerman says that the combination of technical expertise and clinical experience is unique.
“We want to go a step further than one normally does as a researcher in technology, and ultimately create specific practical applications. It is often a problem in the academic world that one is driven by the desire to be published and cited in scientific journals. Far too seldom do we go the extra mile to achieve something that really works at the clinic,” he explains.
The researchers at Linköping are already able to study in real time how a patient’s brain works while the patient is lying inside the scanner. The brain consumes more oxygen in the areas that are doing the most work. The camera can pick this up – if it can manage to count the very small differences that characterize high and low activity.
“We can also see exciting developments in computer tomography. Our new full-body scanner can capture 25,000 pictures in two seconds. They can be combined to form a 3D representation of a human body and be used for visualization. We can also run the machine so quickly that we can take 16 images a second of a beating heart, creating a film of the heart for instance showing how the valves are working, for example,” adds Professor Ynnerman.

Data quantities is a problem
But great technical challenges still remain. The human body is a highly complex system, and the various technologies describe the same phenomenon in different ways. Combining thousands of images of differing kinds is difficult and also demands enormous computing capacity. Good mathematical algorithms and a little discernment are also needed.
“It’s a question of understanding what data is relevant. For instance, we can increase the resolution in the parts of the image where something interesting is happening, as in the transition between tissues,” Professor Ynnerman explains.
If raw data are discarded after an examination, this creates extra storage space. On the other hand, it will not then be possible to carry out follow-up studies. In the future it may be possible to make simulations for an individual patient, which requires an enormous amount of memory. But a simulation need not be saved, and if it replaces other types of data, it may nonetheless be a way to reduce data quantities.

New technology raises new questions
Yet when we finally have a film (3D time sequence of data) of the body’s functions a new problem arises: How can doctors know what they should be looking for?
Professor Ynnerman mentions orthopedics as an example, where the current method is to CT-scan a patient’s knee at a certain angle, which produces standard images in which measurements may be made.
“But in reality we don’t sit still all the time, and with current methods we can have the patient bend the knee during the scan. This gives us images of an entirely new kind; at the moment there are no standards for how to take measurements from them. We have to find new ways to convert the data into something we can document in medical records.”
New imaging techniques may eventually offer enormous potential. It is not just a question of making diagnoses; it is also about prognoses. Professor Ynnerman says that the medical sector has in many ways traditionally had a reactive approach: we have tried to do something about problems when they arise. If we are to better serve an ageing population, we have to be better at preventive healthcare. We have to avert diseases before they occur.
“I have a vision, but it is very much my own, because many people think it is much too spectacular: that medical records across the world are transformed from being a kind of historical document to becoming a virtual copy of the patient. When you go to the doctor, your records are updated and new simulations can be made. We can then see how the heart, brain and blood vessels are doing… But this raises many ethical issues, which must be carefully considered.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström