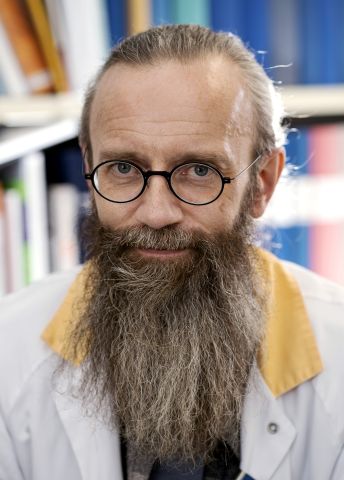
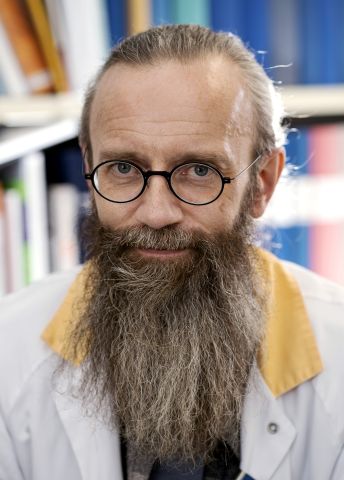
Henrik Zetterberg
Professor of Neurochemistry
Wallenberg Scholar
Institution:
University of Gothenburg
Research field:
Neurochemical tests for pathological processes and damage in the brain

Wallenberg Scholar
Institution:
University of Gothenburg
Research field:
Neurochemical tests for pathological processes and damage in the brain
On the Swedish Alzheimerfonden website it says: “There are no specific blood tests to establish Alzheimer’s disease”. But Wallenberg Scholar Zetterberg and his colleagues are in the process of changing that.
“Alzheimer’s and a number of similar diseases occur when proteins in the brain form clumps, causing tiny inflammations. A protein called beta amyloid forms plaque, and balls of a protein called tau. All this damages the brain cells. In order to treat the protein aggregations and reverse the process, we must be able to monitor what is happening in the brain. And that’s my team’s specialty,” says Zetterberg.
They have spent several years studying biomarkers for brain damage – substances whose concentrations change when damage occurs or decreases. The markers have been found mainly in fluid surrounding the spinal cord and brain, which can be sampled using a syringe inserted between the vertebrae.
“But we’ve recently succeeded in developing highly sensitive blood tests. They’ve really worked well. I never imagined we’d be so successful,” Zetterberg enthuses.
Working with Oskar Hansson, a Wallenberg Clinical Scholar at Lund University, he has compared much more expensive and complicated diagnostic methods, such as PET and lumbar puncture. The blood tests were more or less equally accurate, and are so simple and inexpensive they can be carried out at local health centers.
As yet there are no drugs to combat Alzheimer’s, and it is a challenge for health care workers to carry out blood tests. While the Gothenburg researchers are preparing to systematically evaluate the blood tests, health care personnel need to be trained.
Zetterberg elaborates:
“If biomarkers are to be used clinically, it must be done properly. The worst case would be if someone came in suffering from fatigue and depression for instance, and the Alzheimer’s test revealed biomarkers. That might indicate that symptoms will appear in ten years, but what the patient is experiencing at the time of the test is depression. Things could really go wrong.”
The researchers in Gothenburg are collaborating with international experts to draw up guidelines for how the test results should be interpreted and used. Zetterberg thinks they may be ready by fall 2021 or spring 2022, when the laboratory will be ready.
“It would be of great value if a reliable diagnosis could be made earlier. Best of all would naturally be if we had drugs we could use, followed by further monitoring of the biomarkers six months later to see whether the drugs had worked.
This goal may finally, at long last, be within reach. In spring 2021 the U.S. FDA will evaluate a new Alzheimer’s drug that reduces plaque formation in the brain. The question is whether the drug actually has an effect on the symptoms of dementia: memory, learning, and difficulty in finding words and following reasoning. Zetterberg is not sure the research findings are sufficiently unequivocal. If they are not, he believes that the major pharmaceutical company that has developed the drug will discontinue the project and invest in other options, of which there are several in the pipeline. Here too, biomarkers may play a key role. The primary aim is to find drugs that prevent disease. This requires several thousand patients who have no symptoms but in whom plaque has started to form. Plaque in particular can be detected much more cheaply using blood tests than brain scans. This could accelerate drug trials and reduce costs by many millions of kronor. The biomarkers can also be used to evaluate the effect of new medicines.
“We hope our work will lead to better drug trials. When we have effective therapeutics it will be a huge weight off my mind – it’s a thankless task diagnosing a disease for which there is no treatment.”
Zetterberg and his researchers have now started to address other types of neurodegenerative disease. He envisions a day when we will be able to take a blood test at a health center that reveals our risk of developing dementia, and be referred to a memory clinic or neurologist for treatment, just as today’s blood tests can lead us to heart, lung or liver specialists.
Zetterberg became interested in research in his teens when his father gave him Georg Klein’s book The Atheist and the Holy City. He was fascinated by the story of DNA and cancer, evolution and scientific discoveries. What if he could have a job like that? He began to study medicine, and soon managed to secure a place on a research project.
“Research is so exciting, and it offers a stimulating environment with fun people. I’ve been given to understand that the world of Alzheimer’s research was quite competitive and unpleasant in the 1990s. Many believed they would solve the puzzle, and kept their data secret. But then all clinical trials have ended in failure, so now only the masochists are left. There is much more humility among researchers in this field these days. My impression is that everyone is genuinely pleased as soon as something promising pops up.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Johan Wingborg