
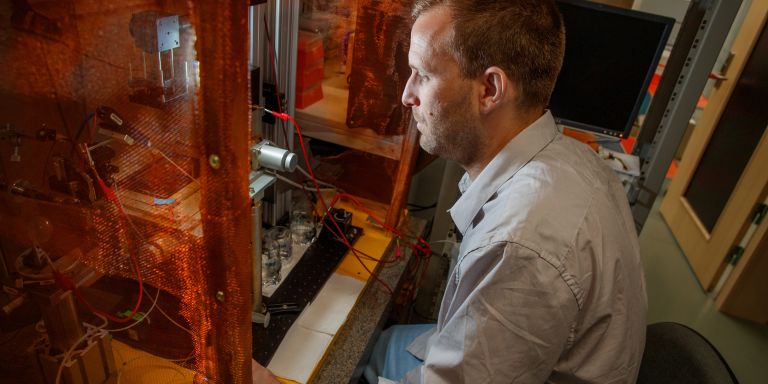
Sebastien Talbot
PhD in Physiology
Wallenberg Academy Fellow 2021
Institution:
Karolinska Institutet
Research field:
The interaction between the immune system and sensory neurons

Wallenberg Academy Fellow 2021
Institution:
Karolinska Institutet
Research field:
The interaction between the immune system and sensory neurons
In his most recent research, at the University of Montreal, Sebastien Talbot focused on melanoma – the most aggressive type of skin cancer. Melanoma tumors contain T cells, which have entered the tumor to fight the cancer cells. Their efficacy declines over time, however, and Talbot has discovered a possible explanation. It appears that sensory neurons grow into the tumor and secrete substances that inhibit the T cells.
“Over time the immune cells lose their ability to battle with the cancer cells, due to a phenomenon known as ‘immune exhaustion,” Talbot explains.
He trained in physiology and pharmacology, but has for many years researched the interaction between sensory nerves and the immune system. Although the two systems are quite disparate in nature and function, they combine to play a key role – helping to protect the body against danger.
The immune system does so by fighting intruders and cancer, the neurons by sounding the alarm when danger looms.
Immune cells and neurons both have surface molecules that are able to receive and secrete signal substances. This enables the cells to interact with each other in what Talbot calls a “local dialogue.”
The nervous system controls the immune system to some extent, and the immune system can regulate the sensitivity of neurons to pain. This dialogue often helps the body, but sometimes it goes wrong. Talbot’s research team has studied what happens to the interaction in a number of chronic conditions such as allergies and inflammatory diseases. They are now focusing on skin cancer.
Though I have made progress in my field, I am constantly reminded that my journey as a researcher has just begun.
The researchers do not yet know exactly how the cancer “attracts” neurons, but they have established that melanoma tumors contain an unusually high number of neurons that can be induced by cancer cells to release neuropeptides, a signal substance. The substances attach to the T cells, causing them to tire and lose their ability to secrete substances toxic to the cancer cells.
In practice the cancer exploits defenses built into the immune system. This is because once the T cells have been activated they have to be regulated so they do not overreact and harm the body. In this case they are instead prevented from fighting the cancer.
“The fact that neurons inhibit immune cells explains the benefit that cancer derives from enabling neurons to grow within the tumor. It should actually be a disadvantage for the disease, since more neurons increase the experience of discomfort and pain, which are warning signals that increase the chances of discovering that something is wrong.”
It has long been known that a tumor can impact surrounding tissue. Tumors can induce blood vessels to grow in between the tumor cells, supplying them with oxygen and nutrients. The same seems to be possible with neurons. Talbot and his colleagues are studying the phenomenon using mice that have been modified so their pain neurons are blocked or marked with fluorescent molecules, enabling their growth to be monitored. The researchers are also using immunological techniques such as single-cell gene sequencing so they can ascertain what proteins a specific cell produces.
“We’ve also begun studies in patients with melanoma whom we are examining to see whether their immune systems are overactivated. This seems to be the case – we have observed the same phenomenon in mice and in humans,” Talbot says.
T cell fatigue appears to diminish in mice if neurons are deactivated or neuropeptides are prevented from binding. It is possible that therapies with this function could enhance the efficacy of the drugs that melanoma patients already receive. Immunotherapy is used to treat severe melanoma. This involves drugs that promote T cell activity, but it does work for all patients. Immune fatigue may be part of the reason.
“Karolinska Institutet has an excellent collaboration between clinical practice and the laboratory, so we have ready access to patient material. This enables me to take my research to a new level.”
Talbot grew up in Montreal with parents who were both factory workers. But he always wanted to be a researcher.
“It’s actually true that I thought about it even as a child. My best friend and I had a chemistry lab in the basement. We did experiments using the kits you could buy. I was absolutely fascinated.”
His parents supported him as he believes working people often do: they were keen for him to have a different life – opportunities they never had. They never insisted he focus on any specific career, but always stressed the importance of school.
“I’m really grateful for all the opportunities I’ve had. Every step along the way feels meaningful when I know that the ultimate goal is clinical tests and being able to improve the lives of patients.”
Text Lisa Kirsebom
Translation Maxwell Arding
Photo Magnus Bergström