Project Grant 2024
A spatially functional atlas of the healing intestinal barrier: implications for inflammatory bowel diseases
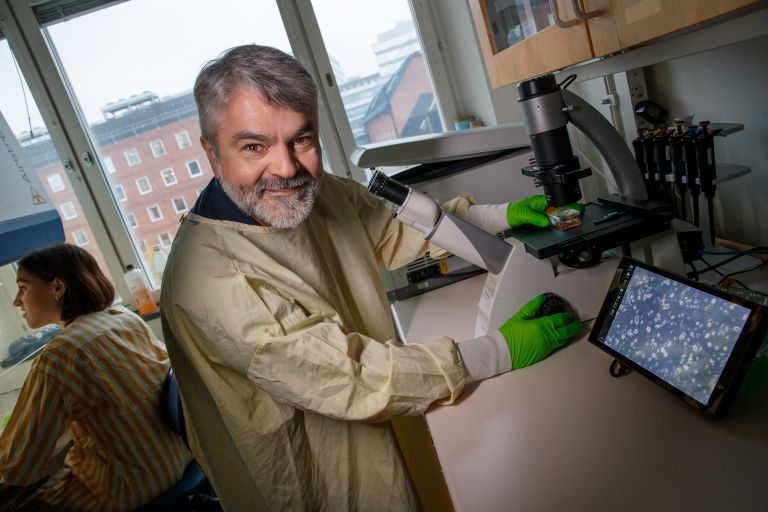
Principal investigator:
Eduardo Villablanca, Professor of Gastrointestinal Immunology
Co-investigators:
Karolinska Institutet
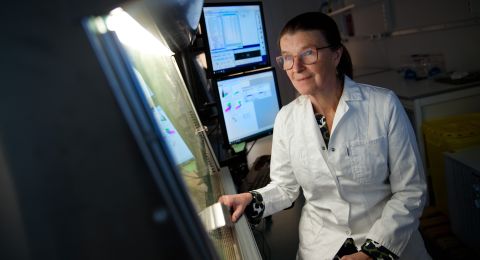
Charlotte Hedin
KTH Royal Institute of Technology
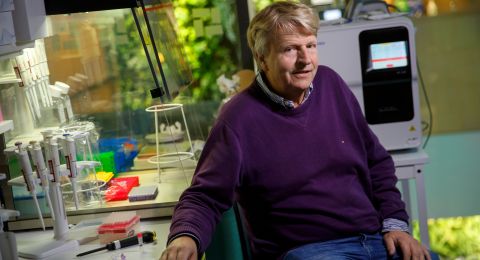
Stefania Giacomello
Institution:
Karolinska Institutet
Grant:
SEK 26 million over five years
It is estimated that some 65,000 people in Sweden suffer from IBD, a collective term for diseases that cause inflammation of the intestines. They include Crohn’s disease, ulcerative colitis and microscopic colitis, all of which cause severe problems, including pain, diarrhea and significant impairment in daily functioning.
“Like most people, I had no idea how much IBD patients struggle in their daily lives. Imagine experiencing stomach pains every hour, constantly worrying about what you eat, and always needing to know where the nearest bathroom is,” says Eduardo Villablanca, professor of gastrointestinal immunology at Karolinska Institutet.
He is leading a research project that has adopted a novel approach to the disease. Together, researchers from three teams will find ways of stimulating the intestinal mucosa’s ability to heal itself.
Immune system on the attack
No one yet knows exactly what causes inflammatory bowel disease or why the condition can sometimes develop into cancer.
“Our immune system is constantly on the go, maintaining a balance in our intestinal environment. No matter what we eat, it adapts. But for some of us, the immune system can suddenly attack our natural gut bacteria, leading to inflammatory bowel disease.”
Researchers have long sought to understand why fewer than half of patients do not respond to available immunosuppressive treatments. For many, the treatment also stops working after a while, and then the only option is to remove the affected parts of the intestine.
As we urgently need alternatives to immunosuppressive drugs, Villablanca’s team propose to stimulate the intestinal mucosa’s own ability to heal. The problem is that no one yet understands how the intestinal healing process works.
“And there is another complication: if we promote healing too much, it can lead to tumors, so treatment has to be tightly regulated,” says Villablanca.
A holistic approach
The project begins with a unique group of patients at Karolinska University Hospital, all of whom suffer from acute inflammatory bowel disease. They are recruited and followed up by Charlotte Hedin, who is also involved in this project. Each patient affected receives individualized treatment, enabling the researchers to monitor multiple pathways in the intestinal healing process.
“We will follow them over a fairly long period to build a comprehensive picture of how healing unfolds. We do this by mapping all the genes, cell types, cell interactions and signaling pathways that contribute to healing.”
The key is to constantly maintain a holistic perspective in the research. Villablanca elaborates:
“We don’t really know what we’re looking for, so to avoid missing key mechanism, we need to capture the communication between all cell types-including interactions with the gut bacteria and fungi.”
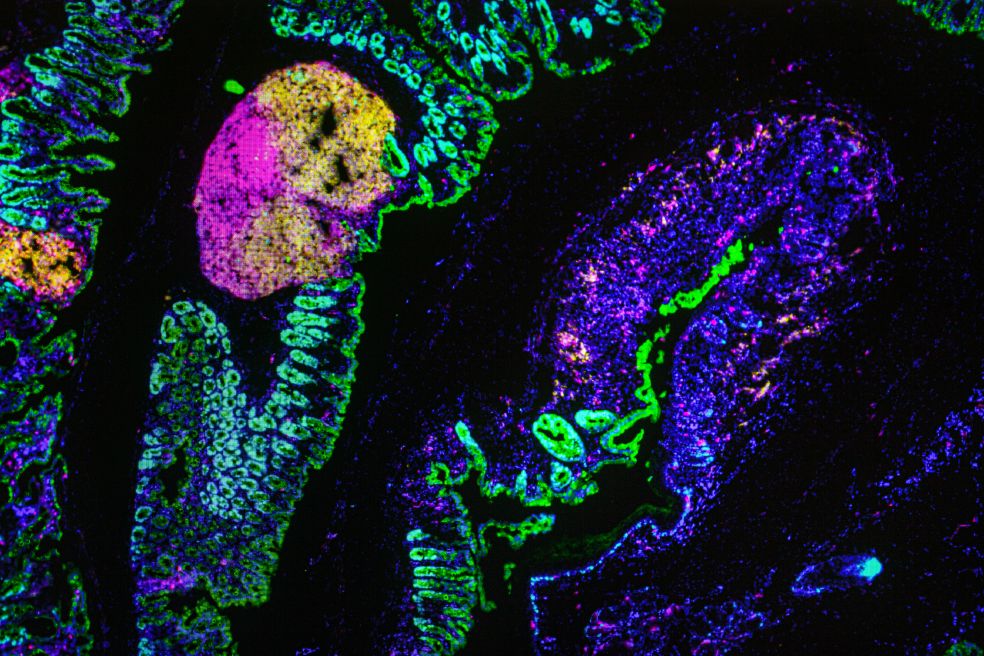
Several advanced techniques are used to collect all the information required. These include single-cell analysis and spatial metatranscriptomics. Simply put, the latter is a development of spatial transcriptomics – a highly successful method of tracing gene activity within their tissue context.
Stefania Giacomello is also involved in the project. She is continuously refining the method so that it not only reads gene activity but also creates a tissue map of the communicating cells.
The tissue map will include interactions between the cells in the intestinal mucosa and also the bacteria and fungi that make up the gut flora. These investigations generate enormous amounts of data and samples stored in a dedicated biobank for in-depth downstream studies.
Tested on organoids
To test the hypotheses that emerge from the data analysis, the researchers are using “organoids”: three-dimensional cell structures that mimic the body’s organs. These mini-intestines are engineered and manipulated to include components of the immune system, allowing the team to model human gut biology with remarkable precision.
“We can then manipulate the intestinal environment in the lab in various ways to validate the patterns we observe in the patient data we gathered.”

The approach is complicated but may lead to groundbreaking results. This was demonstrated at the beginning of 2025, when the researchers published their first article in the renowned journal Nature.
“We identified the first signaling pathway that can promote regeneration while simultaneously inhibiting tumor formation. It’s a clear example of how useful this system can be.”
The researchers found that mucosal healing was promoted when they activated a protein called Liver X Receptor (LXR). The same protein was also capable of slowing tumor growth in colon cancer.
The findings from the project may help not only people with IBD but also those who have undergone radiation therapy for cancer in the abdominal cavity. After radiation, they often suffer intestinal injuries like chronic IBD.
“Our goal is to contribute the knowledge needed to develop future treatments for all those affected. And by improving our understanding of the disease itself, we hope to provide more therapeutic options to patients,” says Villablanca.is
Text Magnus Trogen Pahlén
Translation Maxwell Arding
Photo Magnus Bergström