Antibodies, essential components of the immune system, are produced by B cells. When B cell development is disrupted, it can lead to antibody deficiency or cancers in the lymphatic system. Qiang Pan-Hammarström is working to piece together this complex puzzle, to show how errors in B cell formation can contribute to immune disorders and malignancies.
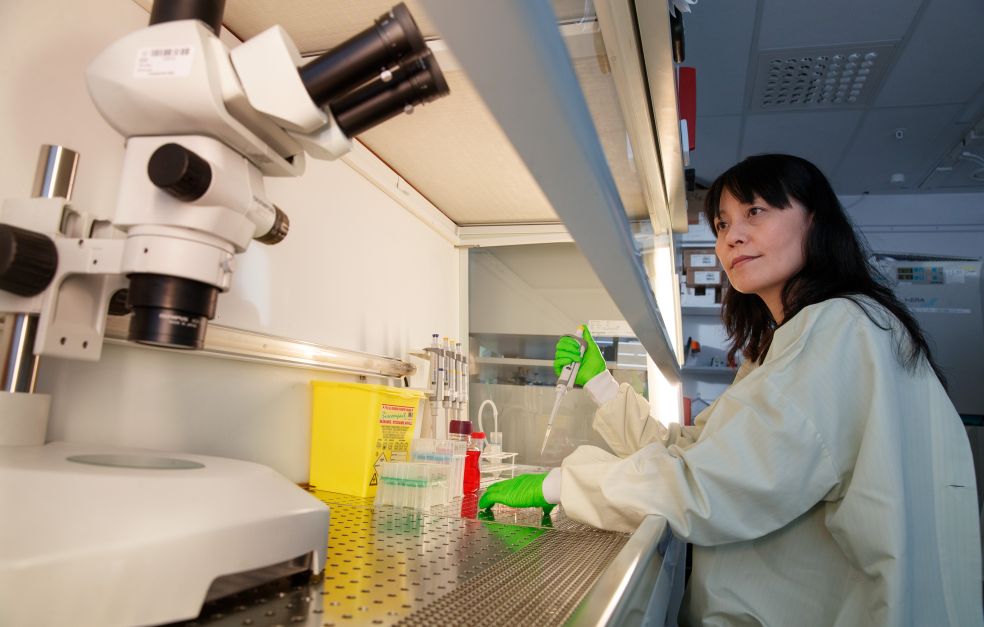
Qiang Pan-Hammarström
Professor of Clinical Immunology
Wallenberg Scholar
Institution:
Karolinska Institutet
Research field:
The role of B cells in immunoglobulin production and antibody deficiency, and in lymphoma
Every day, tens of millions of new B cells are produced in the bone marrow, each capable of creating a unique antibody. These antibodies are designed to recognize and bind to foreign substances, such as viruses. Because each antibody is unique, the immune system can identify and respond to an almost infinite variety of potential threats.
Same genes, different expressions
Each B cell has the same DNA. Despite this, they develop the ability to produce unique antibodies. Wallenberg Scholar Pan-Hammarström began her studies of the immune system during her PhD and is now focused on understanding the molecular mechanisms behind B-cell development.
“It's fascinating to see how well nature works. These cells all carry the same genes, yet through processes like DNA recombination and variable gene expression, they develop unique traits and functions,” she says.
The task of B cells is to patrol the blood and lymphatic system in search of intruders. It was once believed that all B cells were the same. However, a research project funded by Knut and Alice Wallenberg Foundation has shown that many different B-cell subtypes are distributed across various tissues.
Pan-Hammarström is leading the project, which has also broken new ground in mapping B-cell development. She is now building on this knowledge to find out why some people develop antibody deficiencies and cancer of the lymphatic system.
“Our aim is to identify the factors involved in B-cell development, which could help us map the errors that lead to immunodeficiencies or B-cell lymphoma.”
Multiple paths to variation
It is already known that B cells have several ways of generating variations in their DNA. They can rearrange parts of their antibody encoding genes to create new and unique combinations. In some cases, they also introduce random segments, increasing the diversity even further. Additionally, B cells can trigger spontaneous mutations in their genome to refine and enhance antibody functions.
Understanding can yield molecular diagnostic methods that can alert us early on when changes leading to cancer occur. If we identify the right biomarkers for B-cell lymphoma, we can start treatment much earlier.
However, introducing new mutations into the genome is a risky approach. While such changes can result in more refined and effective antibodies, they can just as easily lead to disease. Even gene rearrangement carries risks. If the DNA is not repaired correctly after the exchange, it can lead to cancer. Understanding the molecular mechanisms that govern these processes is therefore a crucial step toward developing new therapies.
Pan-Hammarström sees it as piecing together several puzzles simultaneously and then fitting them together.
“We still lack many of the fundamental puzzle pieces, which is why I am so grateful for the Scholar grant. The funding allows a long-term approach and the flexibility to benefit from new technological advances.”
Different models
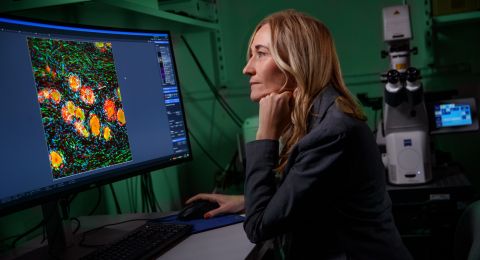
She is using advanced analytical methods that can display gene rearrangement in up to 100,000 B cells simultaneously. This approach provides insights into the active molecules at various stages of B cell development.
Another model involves screening and studying up to 2,000 different transcription factors. Some of these impact cell development in various ways, and the researchers hope to identify the most important ones.
Additionally, “mini-organs” are being grown in the lab. These are based on human cells, with certain genes switched off or mutated.
“We can turn off a gene or introduce mutations that we believe are linked to immunodeficiencies or lymphomas. This enables us to study genes or mutations one by one to see how they affect B cell functions.”
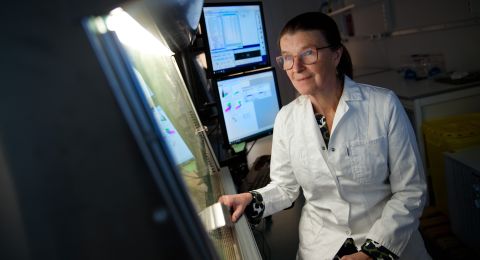
Previous research has largely relied on animal models, which differ greatly from human cells to fully capture human-specific biology.
“We have learned a lot from mice and other animal models, but much of that knowledge cannot be directly applied to humans. By understanding the molecular mechanisms behind these diseases, we may be able to develop new treatments. The hope is to develop new and curative gene therapies, particularly for younger patients.”
Current treatments for lymphoma help about six out of ten patients. The rest do not respond to treatment or suffer a relapse.
Pan-Hammarström’s research is about understanding fundamental mechanisms but also making a difference for patients. Even as a child she knew she wanted to become a doctor — a decision by the tragic loss of her father to stomach cancer.
While working as a doctor in China, she soon realized that more knowledge was needed to help more patients. By chance, a friend mentioned Karolinska Institutet (KI) in Sweden, prompting her to apply for a PhD student position there. Thirty years later, she now works alongside her husband, who is also a professor at KI.
“My husband is also a doctor by training, and we probably talk about research around the clock. We are both driven by a desire to help more patients, particularly those with immune diseases.”
Text: Magnus Trogen Pahlén
Translation: Maxwell Arding
Photo: Magnus Bergström